One of My Most Memorable Medical Mysteries as a medic was a call from a man for his 50ish-year-old wife. On arrival I asked, What’s going on? “She’s just not herself,” he said. Has she been ill? “She had been talking to her doctor who thought she either had a kidney stone, or a bladder infection. She has an office appointment tomorrow.”
Other than that, he said, she had no medical problems, and took no medications. Not a lot to go on, but I went in to see the wife, who was in bed.
Sure Enough
Her husband was right: she wasn’t herself. She was awake, looking at us, even talking, but nothing she said made any sense — as medics sometimes put it, “The lights were on, but no one was home.” She was a bit concerned about all the strangers in her bedroom, but was otherwise cooperative — and confused.
My usual first touch with a patient is to take their pulse: they expect it, it’s non-threatening, and it tells us a lot. But I couldn’t feel it. Sometimes that “just happens,” and sometimes it means problems. Meanwhile, what I did feel was that she was warm; hot, even. It made me worry about something specific, so I grabbed my blood pressure cuff and stethoscope. Her blood pressure was 54 over 38 — she was in shock.
“Shock” Isn’t a Psychological Condition
The more medical name for shock is hypoperfusion: her blood pressure was too low (hypo) to get sufficient oxygenated blood to her brain and other vital organs (perfusion), so no wonder she couldn’t think clearly. Meanwhile, her body had shunted her blood supply away from her periphery to try to get more to her brain, which is why I couldn’t feel a pulse in her wrist.
I told her husband she needed to go to the hospital. “You really think so?” he asked, clearly unsure. Yes: right now.
One of the causes of shock is an infection that’s out of control, and causing systemic breakdown leading to “multiple organ failure” — and she was well on her way.
Getting to the Diagnosis
The husband had given me a hint: possible bladder infection. The result of such an out-of-control infection is called sepsis, which leads to septic shock.
It was a common cause of death before antibiotics. Even now, there are about 20 million cases a year worldwide, and around half the people who progress to septic shock die from it, since the mortality rate rises at about 10 percent per hour once they’re into shock. It’s a darned good thing he called 911 when he noticed his wife was acting strangely.
The only thing we could really do for our patient was to start an I.V. and dump fluids into her to get her blood pressure up a little, as well as simply make her blood less toxic. The medic saying is “Dilution is the solution to pollution.” That, and “apply diesel” — quickly get her to the hospital so they could try to save her with antibiotics and other supportive care in the Intensive Care Unit.
In the News This Week
She lived, in large part because she was otherwise quite healthy. Muhammad Ali, being much older and in declining health, didn’t live through his septic shock: that was his cause of death on Friday. He had bouts with pneumonia and other infections in the past couple of years. He died in a hospital after being admitted for respiratory issues: that apparent infection, even in a hospital setting, got out of control and killed him.
“More antibiotics!” some say. But the rash overuse of antibiotics is part of the problem: bacteria evolve in response to their environment, and medicine can’t keep up with that. That’s why there’s talk of antibiotic resistance, “superbugs” and even “the end of antibiotics” — we’re losing the war due to antibiotic overuse for things like colds and flu, where they don’t work, and feeding low-dose antibiotics to livestock to make them (and their profitability) fatter.
It’s going to get worse before it gets better, so maybe it’s nice to learn about septic shock before someone close to you is diagnosed. Ali’s death is what brought this all to my mind again this week.
All that sounds pretty gloomy, but hey: we saved our patient. May you and yours also be as lucky until the antibiotics problem is solved! Meanwhile, it’s one of the things that attracts me to EMS: I love figuring out the medical mysteries we sometimes need to unravel, which is the first step to getting them healthy again.
– – –
Bad link? Broken image? Other problem on this page? Use the Help button lower right, and thanks.
This page is an example of my style of “Thought-Provoking Entertainment”. This is True is an email newsletter that uses “weird news” as a vehicle to explore the human condition in an entertaining way. If that sounds good, click here to open a subscribe form.
To really support This is True, you’re invited to sign up for a subscription to the much-expanded “Premium” edition:
Q: Why would I want to pay more than the minimum rate?
A: To support the publication to help it thrive and stay online: this kind of support means less future need for price increases (and smaller increases when they do happen), which enables more people to upgrade. This option was requested by existing Premium subscribers.

Good catch. I unfortunately worked with one medic who, when unable get a pulse, would invent one! It took many complaints to get him/her (not saying!) fired. IMHO, unions are great until they protect the incompetent, guilty, or dangerous members.
—
Yep, it’s not about filling in blanks on paperwork, it’s about getting information to guide treatment. -rc
“She’s just not herself” can go in SO many directions.
Kind of like calling a mechanic, to say, “My car doesn’t work”, without giving the details….
—
Yes, but good enough. Sometimes, calling is just a gut feeling, and that’s OK. He wasn’t sure what was wrong, but he knew something was. And he was right! -rc
I appreciate you taking the time to post these EMS stories. Not only are they fascinating and educational, but they allow us to see a glimpse of the people who are our EMTs. Most of us don’t think about you guys until we need you, and then we are too preoccupied to care that you guys are people too. Thank you!
It is only now, more than two years after the fact, that I realized just how close I came to dying from this very thing, and not because I didn’t try to get help either. I had gone to the ER on my way home when I had a growing pain in my back. They dismissed me as, when asked if I had had a fall recently, I answered yes because by coincidence I had fallen the day before, but definitely not hurt myself. I knew I would have to go home and get worse then, which is what happened. My bp was 78/34 when I got to Urgent Care (different town!) and they had a heck of a time getting an IV in. I spent over 24 hrs in the big city hospital ER getting pumped with 10 litres of fluid to get my bp up enough to be admitted. I also heard the word sepsis, but wasn’t aware just how serious that was. Then two days later I get C. diff. from being in the hospital! Ten days after that I was finally released with a super strong, high dose antibiotic to last me another 10 days. I hadn’t known I had a UTI because I am type II diabetic, and the doctor said sometimes diabetics just don’t feel the usual initial pain that you get with that. You were awesome, as was the paramedic that got the IV into me on his first try after all the other pokes I had suffered (at least 12!) before that.
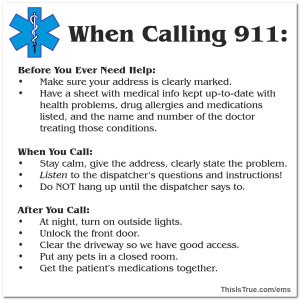
I was saddened to hear that Ali’s death was due to sepsis. That is nasty and makes a person extremely sick before “it’s too late”. Yes, the calls with no information are sometimes worse than saying “motorcycle vs animal” to a trained individual! And thanks for posting the info on “Before/When/After you call 9-1-1”. It’s always a good reminder to be prepared.
Glad your instinct/training told you to get that BP reading quickly, and that you figured it out and got things going. Thanks, as always, for being there for the people who need you.
In January I awoke early extremely tired. I stumble to the bathroom, collapsed on the floor, physically unable to move. Phone was in living room. For 2 hours I lay there not getting any better and vomiting. I finally realized this was NOT going to get better and I had to gather the strength to get to the phone. I finally was able to make it, called 911, too exhausted to barely give my address and condition. I stayed on the phone, the door only 6 feet away, but barely able to get there. Operator kept asking questions, I said if I kept talking I would be unable to breathe. She then said “They are outside your door!” I replied that I was going there, but would take a few seconds. She kept yelling at me they were outside my door. I finally made it, opened it and they took me to hospital. Lungs filled with fluid and pneumonia. 10 days in hospital. Doctor said I would have probably died in a few hours.
All of this story to say: This was scary! I now take my phone EVERYWHERE in house, put a “realtors key keeper” with house key on my front door and will tell 911 operator the combo so they don’t have to break the door down to get to me.
P.S. It was my acid reflex that I didn’t properly treat that caused the fluid build up. Folks the key thing is just a good idea, especially if you live alone. The phone is common sense. And if you have acid reflex, TREAT IT regularly. When it “hurts” it has already done damage. Dr. at hospital who scoped my throat said it looked like someone had taken sandpaper to it. Sorry to be so long. Oh, and I don’t chuckle at those “Help me! I can’t get up” commercials anymore!
As a volunteer first responder (ECA) on our first aid team here at work, I really appreciate your service as a paramedic, and your stories of real-life emergencies. They offer great advice and explanations for those who may miss subtle clues that can lead to a quick diagnosis. We often circulate them at our monthly training refresher meetings. The 911 preparation tag is a great idea, and will be posted here on many bulletin boards.
—
For others, an ECA is a Texas designation: “Emergency Care Attendant”. I’m honored to learn you’re using my stories in your training. -rc
One morning my wife awoke (8:00 am) and her balance was unsteady. We had a Doctor’s appointment for follow up to her hand surgery. Her symptoms did not improve so we made an additional appointment with our family doctor. As we got to the hand doctor’s office two hours later, her balance and coherence had extremely deteriorated. Her answer to questions were off the wall. The doctor did a minor check and suggested we go to the hospital to see if she had a TIA. When we left the first doctor’s office we headed to our family doctor’s office where the appointment was one and a half hours away. Our family doctor could not determine the cause of her problem but said we should go to the hospital across the street. He said he would call an let them know we were coming. It was now after 3:00 pm. Her temperature had not spiked but was beginning to rise as we got to the emergency room. The emergency room staff were great. They diagnosed the problem as sepsis. Her fever spiked to 101.9 while in the emergency room. She was admitted to the hospital where she recovered. The cause: a bladder infection with no warning signs of an infection. Thanks for your story and alerting others of what an uncontrolled infection can do.
Those are all great pieces of advice. What’s your blood type? Allergic to what? Might/Can/Will save your life. I have a list of my medications in my wallet. Seems with every decade I live a add a couple of more. Some, if not taken off of gradually can cause seizures and more. Thanks for posting this. I need to get a envelope with all that info and tack to my front door. I like my combo key container on my front door handle. Even if you have one of those life alert buttons — who is going to open your door for you?
—
At our house, we use combination locks on the doors, and have a “throw-away” code installed that we can give to anyone we want — and replace it if we end up using it. -rc
My Mom died of a massive internal infection back in Jan. 2006 that started & killed her *while* she was in the ICU of a *very* good hospital. Her Doctors did everything possible but the infection was just too strong. So for everyone who says “more / stronger antibiotics will fix everything” I can tell you from *personal* experience that they won’t. No matter *how* strong they are or how much is given, some patients will *still* die from infections. To paraphrase M*A*S*H “there are some rules about medicine; rule #1 is some patients will always die and rule #2 is Doctors can’t change rule #1”.
Thank you so very much for an informative, easy to read, explanation on sepsis. In my line of work (title insurance) I run across sepsis as a cause of death and never quite understood what it was — the explanation I found was not nearly as concise and simple to understand as yours. I also liked the way you tied Ali into it. I have enjoyed This is True for many years and am continually amazed at the stupidity of people. Thanks for putting it together. It’s worth every penny of its subscription.
I use bluestone on my phone. It downloads problem list. Meds, recent Labs, etc right from my doctor. Are EMS professionals told to look at phones for vital info?
—
Only as a last resort, since 1) very few people do this, 2) increasingly, phones are locked — and they should be!, and 3) it’s rare that we have a patient who can’t speak, doesn’t have anyone else who can speak for them, and has information we can find on a phone (and really, in what app? Where can it be found?)
iPhones at least have the ability to put a link to emergency information right on the lock screen, that’s accessible even when the phone is locked — and Google really should build that in to Android, too. Yet most iPhone users I’ve talked to have no idea their phone has that capability, and thus don’t have any information set up to help. One step at a time, I guess….
Meanwhile, I highly recommend — at least for those who have medical problems likely to to lead to emergencies where you can’t speak to us (e.g., diabetes, seizure disorder) that you have a bracelet or necklace from the Medic Alert Foundation — specifically that non-profit rather than the profit-seeking clones — AND keep the information in their files up to date. It’s the best of the bunch to ensure we can get information to help you. -rc
There is hope for the antibiotic problem. Just the other day i heard of something that Europe has used for 100’s of years, but US chose drug companies instead.
Forget the name, but it grows as a bacteria. In some cases they use it just like antibiotics, in other cases, the infection fights it off, so they fake a treatment with it, infection produces what it needs to fight off the attack, then they treat with antibiotics. Since the antibiotic defenses are down during the other attack, they can use much weaker antibiotics. It is in human trials now.
Only took the US a few hundred years to realize the crazy witches knew what they doing.
—
Michael popped me a note later when he remembered the name: bacteriophage — a virus that infects and replicates within a bacterium. -rc
My Verizon phone does have emergency info that can be reached from the lock screen, including allergies, medications, other info, and a short list of contacts that can be called without unlocking the phone. I set it up as soon as I got it, and would recommend that everyone check to see if their phones have it as well. As a single person living alone, I hope that people trying to help me would check it if I was unresponsive.
—
Good to hear that’s spreading beyond iPhones. -rc
I recently recovered from sepsis. It didn’t get as far as septic shock, though close, but it did cause me to faint often. Which resulted in broken ribs. I was fortunate in that the sepsis was caused by kidney stones which had become septic. Yes, I had suffered several months of severe infections before this. I’m 65.
Upon investigating the stones, the urologist discovered the sepsis, so I immediately received treatment. It lasted quite a while. I was fortunate once more in that, when he went in with a laser to destroy the now inert stones, he discovered I had cancer in my ureter. Which I had surgery for earlier today. So, in a way, I was bizarrely fortunate to get the sepsis, though I could have truly lived without it.
But I was horrendously ignorant of sepsis. I suspect most people are. When I told my peeps what was what they were like, “What’s sepsis?” So good on you for at least trying to educate people about the issue. I am an extremely well educated man and, if I was ignorant of sepsis, I’d guess millions more are as well. So speak out man. Trust me, the memory of those broken ribs will ensure I never forget.
—
What a wild chain of events for you. Glad it worked out. -rc
What interested me the most in this story is not the case-study itself but rather your reference to antibiotic resistance becoming a bigger problem as antibiotics are being used too often in situations where they are not really required, i.e. antibiotics kill bacteria but colds & flu are caused by viruses.
I have had a Medic Alert bracelet since 1990 something, when I had my first hearth attack. Each time I arrived in the emergency room (sometimes by ambulance when I was near unconsciousness), no one has ever looked at this bracelet. I heard that there is a law in my state that paramedics, police, hospital, etc. cannot look as it is an invasion of privacy.
I keep updating my my Medic Alert information with allergies, medications and surgeries. If you can’t find your symptoms or problem online a supervisor can change it. I have my advance directive up to date and with me. I plan to give my log in and password to my Medic Alert to my family. I don’t plan to nearly die again. It would be my 7th time. Did you know if you are severely dehydrated you can have no temperature?
—
I don’t think there’s any law against looking at a necklace or bracelet you wear for the purpose of informing the medical profession of your issues, and I’d be highly suspicious of the training of anyone who made such a claim. And you always have a “temperature” — even if you’re dead. Depending on the tool used to measure it, though, dehydration might make it difficult, but not impossible, to measure. -rc
My wife recently took me to the local hospital (against my wishes) because “she had a feeling”. My pulse was 38 and minutes later I was in an ambulance with a doctor in attendance on my way to a major hospital for a weeks holiday.
I am very glad she had that feeling.
Years ago my wife ended up in a major, highly respected, Melbourne hospital after a fall at her work. At about 8pm I was forced to take her home because they said she was perfectly all right even though I strongly disagreed. I put her to bed and got her a drink and found she was bleeding from one ear. I took her back to the hospital, gave the emergency staff who insisted she was perfect a cranal-rectomy (and told them I had called my lawyers).
Within half an hour they found she had a broken jaw and other injuries and that they actually needed to keep her for over a week.
As others have pointed out, your observations for your patient were far better than SOME of your colleagues are capable of. As you demonstrated, “gut feelings” about the well-being of someone you know well should never be ignored.
—
Just to clarify, it was really her husband who had the gut feeling about someone he knew well — he just knew his wife wasn’t right, had no idea why, and called for help anyway, thus probably saving her life. For me it was simply a matter of putting the puzzle pieces together — solving the mystery. I simply had enough experience to narrow it down quickly. -rc
This only works if an infection is not life threatening, but there’s a tool in the ongoing battle against antibiotic resistance. Allimed, a highly concentrated garlic product developed by scientists and MD’s in England; available in the US through a family who almost died of MRSA (Michelle Moore, microbiologist, has a good program to guide people through the process. She’s a member of the BBB, because as she says, doing business online can be scary!). I was able to eradicate my MRSA (it takes several months). It allowed me to save antibiotics for when I really need them (like my recent bout with acute diverticulitis!).
My family and my wife’s family both had to deal with elders who developed sepsis (my father in combination with a UTI).
My fiancee’s mother entered the hospital to be treated for septic shock a little more than a week before our wedding, but still planned on flying from the West Coast to the East Coast afterwards to attend the wedding. We spent a good amount of time convincing her that that was a Bad Idea (TM).
Ever since I heard Muhammad Ali died of sepsis, I’ve wondered if he could have been saved. Did they miss it at the hospital? When I accompanied a friend to the ER a few months ago, I noted that every room, every hallway, in the ER had a sign on the wall reminding the staff to think of SEPSIS. I infer from that that it’s often missed. Do you, Randy, as the one with experience, believe they could have saved Ali if they had recognized his symptoms sooner?
—
I don’t have any information to evaluate on that. But just because someone dies in a hospital from an infection doesn’t mean the hospital is to blame: he could have had it for weeks before he got there, and sometimes you just can’t get on top of it. -rc
Along a similar line, several years ago I was teaching a paramedic class. Mostly young guys in their mid twenties. The scenario was a 41 year old female feeling faint, low BP, but not really shocky, and some diffuse abdominal pain.
We asked them to determine a working diagnosis.
After 15 minutes we called it off. She had a ruptured ectopic pregnancy, and none of these guys thought that women in their 40’s a: Ever had sex and b: could possibly get pregnant.
We ran a similar scenario later that year. That class had a 35 year old. He got it in three minutes.
—
There’s something to be said for experience! -rc
“More antibiotics!” some say. But the rash overuse of antibiotics is part of the problem: bacteria evolve in response to their environment, and medicine can’t keep up with that.
One way, though, that “more antibiotics” is an answer is to find more antibiotics with different mechanisms of action. Antibiotic resistance is expensive from an evolutionary point of view, and in the absence of antibiotics bacteria that don’t spend resources on resistance will outcompete the ones that do.
So the trick is to have enough different antibiotics available that we can rotate through several, and by the time we get back to the start of the cycle, everything that had a resistance to it will have died out.
And yes, I agree antibiotics are overprescribed and overused.
Great catch but I’m sure you felt it was just a routine use of the primary survey and actually doing something based on your findings — despite being frustrated with the limitations on what you could do, the fluids — sometimes you just have to put the body in the buggy and boogie.
I used to ride with two (not at the same time) who would have continued through the entire gamut of secondary stuff before doing anything. They soon learned what they should have absorbed in training: the list of patient assessment tasks is actually in priority order, the findings affect immediate next steps and that treating the patient is more important than completing the entire (mental) checklist.
—
Exactly. Sometimes the right thing to do is “stay and play” — treat them right there. Other times, no matter what, it’s “throw and go” — they need a hospital. The wisdom is knowing the difference and acting on it. -rc
Can you give a recommendation for the brand of combination door locks you and Kit use? I had not considered that option but will be replacing doors this year and will now investigate further and consider your recommendation or suggestions. Thanks.
—
We got the Schlage locks: if you need the door handle too, it’s this one *, or you can choose the deadbolt only. Both just went in place of what was in the door already. They’re a good combination of quality and cost. -rc
I had a diagnosis of sepsis last month. I’d been feeling awful, and my caregiver described me as looking like a wrung-out dishrag.
I’m always reluctant to go to the emergency room, but from the response I get most of the time, I’m pretty good at knowing when I need to be there.
I got there under my own power, and after a number of blood tests, they started giving me an IV antibiotic to clear things up. They admitted me, and I spent two days in their care. On being discharged, I was given syringes of the antibiotic to administer over the next four days. (Fortunately, I had a PICC line installed when it took the nurses at the infusion center five tries to start an IV for my chemo. The day before my last antibiotic shot, the home medical people called to ask when the PICC line was scheduled to be taken out. I replied, “As soon as they cure my cancer and I don’t need biweekly infusions anymore.”)
By the end of the shots, though, I was feeling a whole lot better, and haven’t been using the oxygen they sent me home with.
I guess the bottom line, though, is that sepsis is sneaky, and you can go for a while without realizing you have a problem. I had people telling me I needed to be examined. When I called my mom for the regular weekly call, she told me if she had my symptoms, her neighbors would be dragging her to the ER, by force if need be.
—
For those who wonder, a PICC line is a peripherally inserted central catheter — sort of a super I.V. that delivers drugs to a “central” vein, and is usually left in place for a relatively long period. -rc
I have to comment that my husband rang me at work describing extreme pain in his shoulder. I advised to call an ambulance as I was about an hour away and hospital is 30 minutes, ambulances stationed 15 minutes away. I got home just minutes after he left in the ambulance. Why? Because the Queensland government mapping system has a different road name on their records to the local government and postal service, so we live on the Bruce Highway (longest road in the state) at Etna Creek. They call it Yaamba Road on their system. They have no locality of Etna Creek, listed despite a gaol housing over 800 inmates, being right here 1.4 kilometres away. Goodness jnows how paramedics would ever get there in an emergency. Lastly, on Sundays, the 000 call centre is not staffed locally, but from Brisbane, where the operators don’t know the area.
Ambulance was sent past our place to plentiful Creek road. Hubby heard them go past, heard them go back past. He called 000 again and stayed on the line as he gave directions. Because he was in such pain, and distressed by the ambulance passing by, they arrived to find his blood pressure was 238/160. He was about to explode. Hubby was 75 years old at the time, so not a young healthy person.
We are ever fearful of the same situation happening again. Hubby is now 80.
—
Wow! That’s a severe blood pressure. Glad he survived. Definitely speak with local first responders to ask how to get them there directly if there’s a “next time.” Saying it’s 1.4km (N, S, E, W, whatever) from the prison would probably help. Good luck! -rc
We do tell everyone that, but Brisbane didn’t pass that message on to the driver. The paramedics were very apologetic and thanked him for giving directions the second time.
—
Dunno if Qld has “mile markers” (sign posts along the highway, in your case probably more likely km markers), but that’s another way to give a location. “XX highway, also known as YY road, at mile(km) marker 23.8.” In my county, the addresses are assigned according to the mile marker on county roads; the house number at MM 1.0 is “1000”, so as long as you know where the road starts, you know that #1528 is 1.5 (and a little bit) miles up the road. It’s pretty helpful to me as a first responder. -rc
Is that the same, or different, from hypovolemic shock?
(Yes, I watch too much medical television…)
—
Different (but a good question). Hypovolemic (too little in the “volume” or space) is what happens with heavy bleeding. If it’s due to severe dehydration, it’s similar to sepsis in a way, but from a different reason, and without the “toxic” compounds in the blood. -rc
My mom suffers from UTIs and one of the first symptoms I notice is her mental state becomes off.
—
Look into the supplement d-mannose, a type of sugar metabolite. It was recommended to my wife for a cat that had recurrent UTIs. We get it in powder form and put about 1/2 gram in each of our cats’ water, and haven’t seen a UTI in them since. You can get it from Amazon in capsule form too (affiliate link). -rc
Our house has its number, our mailbox in front of house has its number…but one night the pizza man could not find our house, which let me know that emergency services might have a problem. Ended up getting one of those big green plaques with the reflective numbers to put on end of carport.
—
Excellent! -rc
I remember when you first posted this. Now it’s hit home. My hubby got a UTI in Dec. It spread to his kidneys; I forced him to go to the ER. Still under covid rules, so I left him at triage. He was in ICU a week. In Aug I did it too. Sepsis sucks! Trust your gut.
—
I’m glad YOU did! -rc
Neurologists are beginning to prescribe it for MS patients, too. It *can* cause issues with blood sugar for diabetics, though, so that’s something to look out for.
—
Yep: indeed it’s a sugar, but used in quite small doses. -rc
I’ve had septic shock. I’ve been through MOF. It is not something I would wish on anyone. Mine was a result of allergy to a pain medication the docs gave me for a previous surgery. No one found out until after I had died and been resuscitated in the ICU, with machines and medicines all turned off. No one knew anything until after I had recovered and released, I used the pain medication again for hurting my knee, then when I went for the blood test, they told me I was dying again. M wife and I put two and two together, looked it up…. allergy.
My end result: 1 month in hospital, 4 days in coma, total amnesia from the time I went to the doctor to the time I woke up from the ICU. And the whole time while in septic shock I was incoherent, confused, super low blood pressure.
I got lucky. So did she. Not many others do.