In This Episode: “Doctor knows best,” the saying went. While delivered as reassurance, its real meaning was much more sinister, as I’ll explain. This is the story of the final nail in that idiom’s coffin because really, it was a lie all along. The crazy thing is, that didn’t happen all that long ago.
089: The Deserved Death of “Doctor Knows Best”
How to Subscribe and List of All Episodes
Show Notes
- Help Support Uncommon Sense — yes, $5 helps!
- Update: Robin Warren died 23 July 2024 at 87.
Transcript
“Doctor knows best,” the saying went. While delivered as reassurance, its real meaning was much more sinister, as I’ll explain. This is the story of the final nail in that idiom’s coffin because really, it was a lie all along. The crazy thing is, that didn’t happen all that long ago.
Welcome to Uncommon Sense, I’m Randy Cassingham.
When I was a kid, it was common knowledge what caused stomach ulcers: spicy food; stress, especially from overwork; excess stomach acid.
The first doctor to describe gastritis, the stomach condition that leads to ulcers, was the “Father of Medicine” himself: Hippocrates, in around 400 B.C. Yet it wasn’t until 1868 that German physician Adolph Kussmaul found a treatment that worked pretty well: compounds containing the element bismuth, which is still used today — it’s the active ingredient in Pepto Bismol, a trademark for bismuth subsalicylate.
But even in the 19th and 20th centuries, doctors were still at a loss as to the cause of ulcers, which are found not just in the stomach, but also the duodenum, the upper part of the intestines that the stomach empties into. They suggested non-specific “chemical factors.” Russian doctors suggested infections.
In 1881, microbiologist Theodor Klebs suggested bacteria was the cause, as might be expected from a microbiologist. But that was doubted by many doctors, and was finally fully shut down in 1954 by a large-scale study by a gastroenterologist, Dr. Ed Palmer, which he said proved there were no bacteria in the human stomach whether the person had gastritis or not. The idea: bacteria just couldn’t live in the acidic environment of the stomach.
“These findings, supported by the efficacy of antacids,” said biologist Carl Bergstrom of the University of Washington, “supported the alternative ‘chemical theory of ulcer development,’ which was subsequently canonized.” So there you go: medical canon was “chemicals” caused ulcers, but of course we still knew spicy food and stress at least made them worse, right?
In 1971 a new drug was introduced to combat ulcers: Tagamet. It’s actually an antihistamine (an “H2 receptor agonist”), which inhibits the production of stomach acid. Because as westerners moved into the industrial era, with increasing on-the-job stress, the incidence of ulcers skyrocketed. Pretty much proves the stress theory, right? Well, Tagamet to the rescue! It was approved in the U.K. in 1976, and in the U.S. in 1979. Even though its side effects included diarrhea, rashes, dizziness, fatigue, constipation, muscle pain, mental confusion in the elderly, and even rare cases of loss of libido, erectile dysfunction, and gynecomastia in men, it became the first-ever “blockbuster drug” — the first drug to break the billion-dollar-per-year revenue level for its manufacturer.
My wife’s father struggled with an ulcer that bled so much that, in 1961, he needed 32 units of blood to keep him alive. Doctors froze part of his stomach and, when that didn’t help, they cut out two-thirds of his stomach, which meant for the rest of his life he could never eat very much at one sitting. He was told to be sure to eat plenty of cheese, because dairy was soothing to ulcers. While the blood transfusions saved his life they also, he discovered years later, apparently gave him hepatitis C. But he still almost made it to his 94th birthday.
The problem with the story so far is, the medical canon — or “prevailing dogma,” if you will — was totally, completely, wrong. Stress doesn’t cause ulcers. Spicy food doesn’t either. And dairy makes them worse, because dairy promotes the production of stomach acid.

In 1981, Dr. Barry Marshall started an internal medicine fellowship at Australia’s Royal Perth Hospital, working with a senior pathologist there, Dr. Robin Warren. The problem with Tagamet, Dr. Marshall said, was “as soon as [patients] stopped taking their drugs, the ulcers came back.” In other words, the drugs may help the symptoms, but they don’t cure the disease.
When doing biopsies, Dr. Warren (the pathologist) had noticed that people with gastritis and ulcers had a lot of bacteria in their stomachs. The project he decided to work on with Dr. Marshall during his fellowship was to figure that out: according to Dr. Ed Palmer’s study from 25 years before, bacteria can’t survive in the stomach.
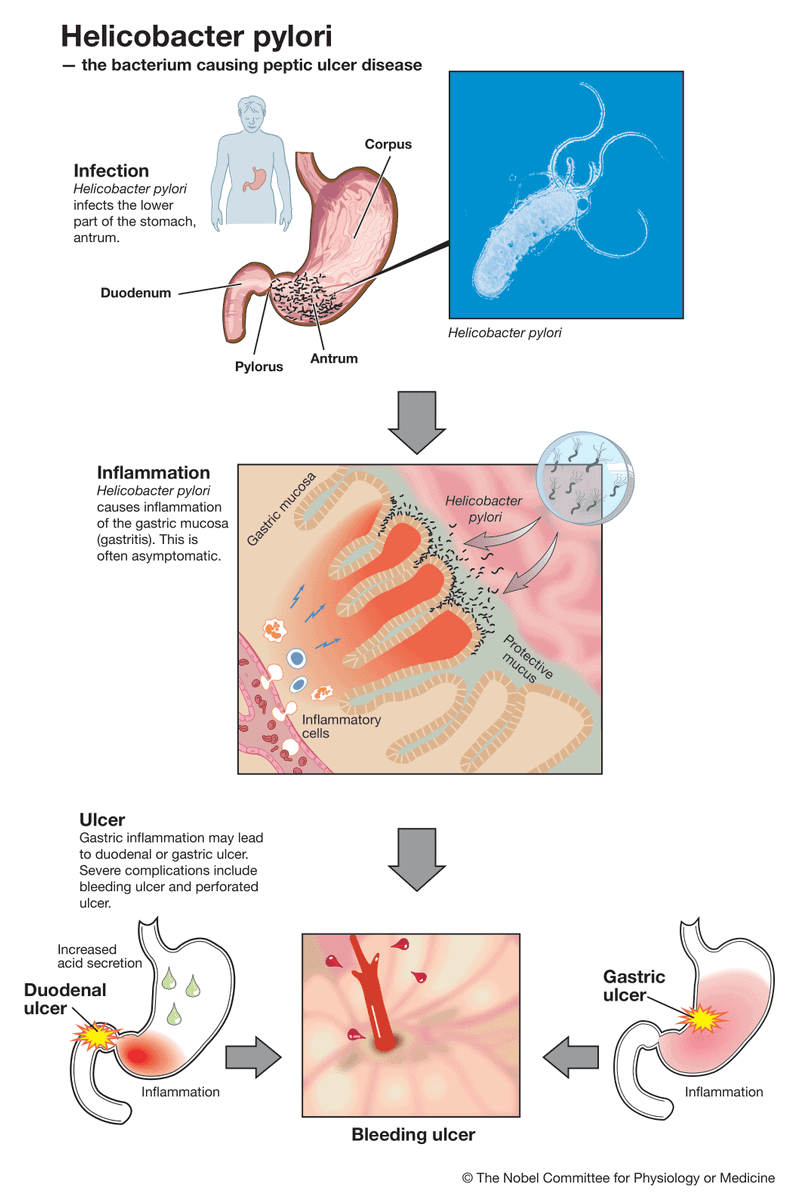
They got a grant that would support their research, and got to work. The goal: to prove that bacteria can live in the stomach, and try to find out how. And sure enough, they found that in people with objectively diagnosed gastritis, there was bacteria in the stomachs of 95 percent of them. What’s more, Dr. Marshall realized that it was a new strain of bacteria that hadn’t been identified before; it was eventually named Helicobacter pylori, or H.pylori for short.
Dr. Palmer, Marshall and Warren realized, was wrong, and here’s how the bacteria can live in the stomach: they just hide under a layer of mucous that protects them from stomach acid.
So how do we treat bacterial infections? Antibiotics.
“I was starting to treat a few people with antibiotics,” Dr. Warren said, “and nine out of 11 seemed to be cured. At the time, the cure rate for ulcers with any other treatment would have been one out of 11.” The problem was, that’s anecdotal evidence, and the gold standard in medical science is a double-blind controlled study, which means there is a control group that’s given a placebo, a test group given the experimental treatment, and neither the doctors nor the patients know which group they’re in until the results come in, and the groups are, as they say, “unblinded.”
But that’s expensive, and their grant money was running out. Experiments on piglets were inconclusive — it turns out pigs have pretty much cast-iron stomachs, which is what I would expect from pigs! — and the granting agency was pretty much like the rest of the medical profession: they didn’t believe these two guys were right. In 1983 the Gastroenterological Society of Australia rejected Marshall’s pitch to present his research at their next conference, ranking his paper in the bottom 10 percent of the submissions.
But the British journal The Lancet published a letter where Warren and Marshall described their findings, and teams all over the world got to work to see if they could replicate their findings. Sure enough, the next year the Gastroenterological Society of Australia accepted their research paper for presentation at their next conference.

Still, most doctors were dubious until what one writer called the “Mad Scientist” approach, and what I call relying on a very interesting strain of Uncommon Sense: in July 1984, Dr. Marshall looked at a beaker of goo grown from cultures taken from patients’ stomachs — a slurry of H.pylori — and, he admitted later, “drank it down in one gulp then fasted for the rest of the day.” The next day, he felt fine. But a couple of days later, he began to feel ill, and a couple of days after that he started vomiting most of every day.
Meanwhile, he had Dr. Warren take regular samples from his stomach lining. Marshall remembered during one of the tests, his boss said, “Barry, I’m not sure why you asked me to do this test on you, and I don’t want you to tell me.” The objective diagnosis: Dr. Marshall went from perfectly healthy to having severe gastritis in just a few days. After two weeks of tests, Dr. Marshall prescribed himself antibiotics, and just as quickly made a full recovery, proving the thesis: H.pylori caused gastritis, which causes ulcers, and antibiotics can cure it.
“When you start off with a new idea like this,” Marshall said later, “all your scientific pals set out to prove you wrong.” But that’s OK, he says: “That’s the scientific process. In my case, people were especially interested in showing that I was wrong, because at the time I was not at the pinnacle of gastroenterology, or even in the mainstream. I didn’t know all of its secret teachings, if you like. I would just charge in with this stuff about bacteria, and nobody wanted to be told that they had spent their life doing research on something that somebody in western Australia figured out in 12 months.”
He thinks skepticism was the least of the problem in their theory being accepted. “I think there was a strategy in the pharmaceutical industry to keep the new bacteria theory of ulcers under wraps,” he said. “At the time we made the discovery, a new antacid was coming out every year or two that was stronger or better in some way, and as each drug was rolled out, the pharmaceutical companies funded scientists to do clinical studies on people with ulcers.”
The thing is, those scientists were paid to prove the drugs helped, not to show that ulcers could be treated by generic antibiotics. “If you look at it from a business point of view,” Marshall said, “it could only do your market harm and lower your share price to find out that you could actually cure people with antibiotics.”
But why take such drastic action of infecting himself with H.pylori? “We felt it was important to act,” Marshall said. “Maybe it would have been different if we’d been talking about [a cure for] a skin rash or something; maybe you can afford to wait five years until that’s proved. But people died from ulcers,” he said, “and were having their stomachs or half their stomachs removed; there were permanent, mutilating operations and deaths going on around us. And yet to test our idea, you just needed to take some antibiotics. So we weren’t very ashamed about trying to get our message out, even though it was rather preliminary.”
That’s thinking with Uncommon sense. Well, not only did formal studies prove them right, in 2005 Drs. Warren and Marshall shared the Nobel Prize in Physiology or Medicine for their work, which has improved millions of lives, and saved hundreds of thousands from a painful death.
See, the real issue with “doctor knows best” wasn’t that it was reassurance to nervous patients, it was actually a message of “just shut up and do what I tell you,” delivered by doctors made arrogant by the prevailing dogma. It wasn’t that long ago that doctors made decisions for you — they often wouldn’t even tell you if you had, say, cancer. But what makes the idiom really sinister is that there’s another way to express the same idea: “This is the way we’ve always done it …(because everything else we tried didn’t work).” And I think Drs. Marshall and Warren put the final nail in its coffin, and rightly so. Patients have a right to make their own decisions when it comes to their health, and the attitude behind “doctor knows best” doesn’t allow for that.
And here’s my evidence that Dr. Marshall’s Uncommon Sense wasn’t a one-off fluke: his work, “was definitely a paradigm shift,” he said in an interview a few years after his Nobel Prize win, “because it got this stress thing debunked. And the implications of that are much bigger: What else is supposedly caused by stress that we can debunk? A lot of these things that are supposedly caused by stress, you try to track down the reason for that link, and there isn’t one, except the fact that we don’t have any better cause [to blame]. Everything that’s supposedly caused by stress, I tell people there’s a Nobel Prize there if you find out the real cause.”
The Show Page for this episode is thisistrue.com/podcast89, which has photos of what H.pylori looks like, and what Drs. Marshall and Warren look like. There’s also a place to comment.
I’m Randy Cassingham … and I’ll talk at you later.
– – –
Bad link? Broken image? Other problem on this page? Use the Help button lower right, and thanks.
This page is an example of my style of “Thought-Provoking Entertainment”. This is True is an email newsletter that uses “weird news” as a vehicle to explore the human condition in an entertaining way. If that sounds good, click here to open a subscribe form.
To really support This is True, you’re invited to sign up for a subscription to the much-expanded “Premium” edition:
Q: Why would I want to pay more than the minimum rate?
A: To support the publication to help it thrive and stay online: this kind of support means less future need for price increases (and smaller increases when they do happen), which enables more people to upgrade. This option was requested by existing Premium subscribers.

I’m old enough to remember going to a dr. and asking questions and having him (was always a him in those days) pat my knee and saying, “Don’t worry about that. I’ll take care of it.”
Yeah, that was pretty much the wrong thing to say to me. I just kept asking until they answered and of course, figured I had no idea what they were talking about. But I sure knew how to read a book and I would look up stuff and have more questions the next time. Doctors were trained to think of themselves as gods and all the patients had to do was obey.
—
Yep. What you describe is pretty much the wrong thing to say to anyone, and it’s about time that the profession, in general, has gotten that message. The humiliation over ulcers (among other wake-up calls) finally forced changes. -rc
The other scary part is that “the experts” may have hidden incentives that push them to find particular answers. Some are obvious: doctors employed by tobacco companies have a strong incentive to find cigarettes harmless or even beneficial. But where else might there be such incentives? Experts studying the crisis du jour, whatever it might be, might well have an incentive to show that the crisis is severe (and so they need more funding to study it).
I’m not saying that any particular expert is acting on those incentives… but the cynical side of me always has to wonder.
There was a study done, published in Lancet last year, on a particular potential treatment for Covid. Short synopsis, the article was explaining why a particular treatment could not possibly work and was dangerous to try (despite the fact that it is safely used for an unrelated issue).
A friend of mine told me about it. He was one of many who wrote Lancet with evidence that this research was flawed. A few weeks later, Lancet repudiated the article — among other reasons, because some of the people promoting the flawed work had strong ties to companies with alternative and much more expensive treatments for Covid…. So, yeah. Money talks.
—
And thanks to checks and balances, the article was repudiated and the authors’ reputations damaged. Excellent. -rc
I was diagnosed with “stress” when I had debilitating abdominal pain my last summer in college. I couldn’t understand how that was possible, given that it was summer break. Turned out to be a massive ovarian cyst which required surgical treatment.
—
Seems to be a convenient catch-all that they like better than “I don’t know.” Glad it wasn’t an even more serious condition. -rc
And I just have to feel that if you had been male, the doctor would have jumped all over himself to get a diagnosis. There is still so much bias in medical decisions whether the patient is male or female.
I don’t know about the attitude/gender bias; I do know that only comparatively recently the medical profession and pharmaceutical industry woke up to the fact that men and women often DO NOT present the same symptoms or respond to the same treatments (even though I’ve seen a man with PMS, too). In other words: there IS no “one size fits all.”
—
The “classic signs of a heart attack” are based on men; women often present very differently, and I have no doubt many died over decades because their symptoms were not considered serious. -rc
I choose doctors by:
1) if I have nothing else to go on, I will choose a woman over a man for two reasons: (a) she is the product of a more darwinian process, and (b) she will probably listen to me.
2) If I need surgery, or any other invasive “procedure”, I ask the doctor whom *they* would chose. They know each other, so they can make an informed choice. So far, my system has worked.
As far as Drs. Warren and Marshall: Well done! Follow the science and conduct experiments. Y’all have changed the world in a positive manner.
—
Your strategy mirrors mine. I got a doctor in southern California when I had to go into the E.R. to get stitched up. I asked a nurse who was a really good doctor in town, the sort she likes to work with. She said she wasn’t allowed to say, but handed me a list …with her finger on one particular line. I thanked her and called the number on that line the next day. -rc
I forgot to add one other thing. I want a doctor who will say “I don’t know”. That is a legitimate answer. I find a woman doctor is more willing than a male doctor.
One (light) sidetrack: I have often been puzzled why a woman would go to a male gynecologist if given a choice (I know…). The plumbing is different enough, and *much* more complex in a woman, that a male doctor cannot grok all of the subtleties. I am sure there are good male gynecologists, but there seems to be a cognitive dissonance. Perhaps I am overthinking this.
—
We’re similar again: I argued (in, surprisingly, Make Cheating Wrong Again) that I want doctors who look it up when they’re not sure. They certainly can’t remember it all — not anymore. And yeah, if I want female doctors, I’d think women would have that inclination several times over! -rc
Agree with you wholeheartedly about women going to a male gynecologist? Don’t understand the logic — or lack thereof. It does not matter if a male doctor is educated in the world’s top medical academy & taught all the medical sciences! He just cannot, in any way, know the many nuances associated with the female body & the associated reproductive process, not having either!
P.S. Enjoy This Is True; and love your writing style RC!
—
Thanks, Beverly! -rc
I am a retired family physician. My medical school class was 15% female; we were just starting the upswing. I had specialists tell me I was good enough to go into their specialty; why was I choosing to be “just” a family doctor? I subscribed to the philosophy that I was a teacher (doctor and docent come from the same root) and a partner in decision making. A few patients really wanted me to make the decision, but most were happy to be given some choice. I was also told that the “half-life” of medical knowledge is 7 years: in 7 years half of what a doctor “knows” will be proven wrong. The problem is that we don’t know which half! That kept me humble. I had a good life as a family doctor, though I never got rich. The relationships with patients were what made my life fulfilling.
—
You’re my kind of doc — bandit’s too, I’d guess! -rc
For years I avoided all avoidable contact with doctors after one (a woman MD) stared as though I were a cow who had learned to speak — because I asked a pertinent medical question. Conditions have improved since then and I have a good MD now, but most MDs are the products of medical schools who may be substantially endowed by pharmaceutical companies. One more reason for modern distrust of ‘conventional’ medicine.
I was reading through these comments again when I arrived at this, and laughed inwardly about my last physical: my doc was rendered speechless when, speaking of my allergies, I said I “alternated between loratidine and fexofenadine” — he had to think about it to translate that to “Claritin and Allegra”! I said, “I thought you all were trained now to use generic drug names?” Yeah, well, old habits die hard.
Back about 1980 I was having some stress at work and had severe stomach pains. Naturally the doctor diagnosed me with the beginnings of an ulcer and gave me a prescription, plus advising antacids. So I started popping antacids like crazy to survive, until one day I spot a tiny article on the back page of the newspaper. It explained how some people were found to be sensitive to sorbitol, a sugar alcohol used as a “sugar free” sweetener. I investigated and found it in the mints that were new and I had bought a big package of them on an introductory sale. Problem solved. Also, I realized that sorbitol had nearly as many calories as sugar, so it was not a good substitute. I have not had stomach pains like that since, and it’s been decades since that brand of mints completely disappeared from store shelves.
Sorbitol is still used in many, but apparently in lower levels than those mints, and I mostly avoid it, and especially in the amounts taken for those couple of months. Sometimes we have to watch out for ourselves.
—
I think we always need to watch out for ourselves, and investigate/get a second opinion when the doctor’s advice doesn’t help. -rc
While I’ve been around some doctors who are the “Shut up because I know better” types, the most egregious one was when, after a concussion, he had given me pain pills (Tylenol 3) for the headache and sent me back to work. Three days later, the headaches still hadn’t gone away and I noticed I was having trouble with my vision as well. Normally 20/15, yet I was having problems writing small enough on the cels I was drafting on. So I went back to the Dr and he tossed me another pain pill prescription. I brought up my vision and he tested it at 20/40. I told him that was wrong, but he just patronizingly told me it must have been a slow change that I didn’t notice. Like close work, drafting, snuck up on me? I don’t think so. Well, I got to thinking that night … Concussion -> swelling -> acetaminophen does nothing for that -> aspirin does. Switched to Excedrin and the headaches were gone by the end of the next day and my vision was back to normal.
A more recent one wasn’t so much my Dr. being above it all, but a more normal lack of knowledge, although it would have been better to say he didn’t know. I had Guillain-Barré Syndrome (an auto-immune paralysis that attacks your own nerves which can kill and can be triggered, although they don’t know how, by the flu or a flu vaccine shot — it was a Swine flu vaccine that year) when I was 20, and flu and pneumonia shots are contraindicated (although the advice on that is changing too). So the COVID shots were valid reasons to worry, especially when there were at least two GBS outbreaks that seemed to be associated with COVID. When I first brought up the vaccine with my Dr, he wanted me to wait for the Astra Zenica one (I guess he thought that would get out before the J&J). But I did a lot of digging and came to the conclusion that an mRNA shot had a far lower chance of triggering any auto-immune response since it only dealt with one, single, individual protein rather than a full viral RNA strand of any kind. GBS is rare enough that he may well never have had a patient or even knew someone who had had a patient who had ever had it. But people really need to know enough or be willing to learn enough, to make some decisions for themselves, even, or especially, when the doctor may be innocently wrong.