Something fairly profound happened to my wife and me Sunday. I have a group of friends that I communicate with regularly via an email list, and Sunday afternoon I shared what happened with them. One asked, “Great story. Will you be sharing it with your readers?”
Hm: good question. I said I was pondering it — but I don’t very often tell stories about my volunteer EMS experiences in my weird news newsletter, yaknow?
“Good News Helps”
Another piped up: “Do it. People need good news right now. Especially some of us who are getting nervous as 50-somethings around us are dropping. Mortality is weighing quite heavy on some. Good news, firsthand accounts of honest to goodness good stuff helps.”
He was referring to a number of recent well-publicized deaths, like Michael Jackson, who just dropped dead at 50. The same day, 1970s icon Farrah Fawcett died from cancer. At 62, she was a bit older than 50-something, but that’s pretty close. And yesterday “Pitchman” Billy Mays died too, also at 50.
My buddy is 50-something himself; he’s one of the “some” he spoke of who’s feeling mortal as people around him are dying in, it seems, droves.
The Story
So at the risk of sounding too proud of the “honest-to-goodness good stuff” that happened on Sunday, here’s what happened.
As many of you know, my first career was in EMS — I was an advanced life support medic in between stints as a police cadet and sheriff’s deputy. After getting my degree, working for NASA’s Jet Propulsion Laboratory for a decade, and then going into writing and publishing — a 22-year hiatus from EMS — I recertified as an EMT.
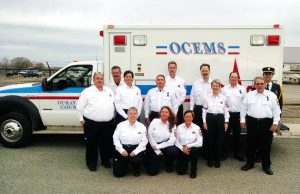
Trained medics were (and still are) in short supply in my rural community in western Colorado, just as in many rural communities everywhere, and experienced ones even more so. Because I have experience, I was given the task of re-establishing a First Responder Corps in my county; a previous team had gone defunct before I moved here.
In my area in Western Colorado, it takes 20-25 minutes for an ambulance to arrive at an emergency, and even that assumes good weather. I now have a team of a half-dozen trained people who can respond at the drop of a hat to help keep people alive in an emergency until the ambulance or the duty paramedic gets there to take over.
Motley Crew
There’s a school bus driver, a church secretary, a retired high school science teacher, a retired U.S. Forest Service guy, a retired county commissioner, my wife, and me.
As the Captain of the squad, the guy with experience, I’m expected to roll on every call to back up the less experienced team members. Knowing I’m coming gives them the confidence to roll into sometimes terrifying circumstances after their (as little as) 110 hours of training.
My wife, Kit, got certified as an EMT at the same time I did: she wanted to do something about that shortage of medics too.
Since I was re-certifying at a lower level than before, it was easy for me to blow through the class. I read the book, but didn’t have to study, even though a lot of things have changed in the 22 years since I moved on to my next career (and I forgot a lot of the things that didn’t change!)
Since we both have to work for a living, the class time was in addition to our busy schedules. It made for 70-hour weeks for me, but Kit had to study on top of that. And she did it, passing with flying colors. On Sunday, I was grateful to her dedication to really learn it.
“Hi, Steve!”
We’ve run some pretty hairy calls. I pulled a little girl into my own car to meet the ambulance, with Kit driving us out to the county road from the girl’s rural house to save about 15 minutes to meet the ambulance, because the child was in status epilepticus (a seizure that won’t stop, which is life threatening).

We arrived at a wreck, and I looked down at the driver lying on the ground, and my first words to him were, “Hi, Steve! How’s it going?” — someone else I knew, and it was a miracle of timing that he hadn’t been killed when his truck rolled over and the roof collapsed to his shoulder level. He had been thrown out of the way just as it would have crushed his head. He walked away with a broken arm.
This week a neighbor we know had her horse fall on her, slamming her head into the ground so hard she asked what happened again and again — about 30 times — while we waited for the ambulance to arrive; her memory simply didn’t work. Each time, after Kit or I told her why she was lying in a pool of her own blood, within 5-10 seconds she couldn’t remember the answer.
And a couple of years ago, another neighbor we know was lucky to survive when a big-rig tow truck slammed into him …right in front of our house.
But all those people survived because they were lucky, not because of anything Kit or I personally did. The call on Sunday, however, was different.
Sunday Morning
We were awakened by my pager at 1:04 a.m. The report: a 50-year-old man, unconscious, about 5 miles away from our house.
Kit’s proud that she can go from asleep to dressed and in the car ready to roll within a minute, even though she has to slap in contact lenses to be able to see. As usual, we were rolling within a minute after Sunday morning’s page.
As the garage door was going up, we got an update from dispatch: “CPR in progress.” Gulp! It’s about the worst news you can get: your patient is dead. You’re going to be there first, you’re going to be there by yourself for at least 10 minutes, and your job is make death a temporary, not a permanent, status.
No pressure there, eh? His only hope, when we’re a good 9 minutes away, is that the CPR is being done well.
Planning Ahead
As we rolled we discussed our initial attack: Kit would go in first and make sure things were under control and progressing toward restoring the man’s life while I gathered up the equipment we needed and followed her in.
As Captain, one of the few defibrillators we have is kept in my car. You’ve seen the “paddles” TV medics use to shock people whose heart has stopped? That’s a defibrillator. I hadn’t used one in more than 25 years. But it’s been in my car, in case I needed it, for several years. I never needed it, but I sure did now. I had just checked it last week, too.
Response Delayed
The first problem hit before we got there. We found the road just fine, but there were no address signs. Driveways tend to be about a quarter-mile long around here. I tried one, but that wasn’t it. I hoped it was the next driveway, and it was. But about two minutes were wasted right there. I pulled up to the house and the patient’s frantic wife led Kit in.
I was less than 30 seconds behind, and entered the man’s bedroom to find Kit on the floor with him, doing CPR. The man’s daughter had done it while we were on the way, keeping him going until we arrived, and Kit had taken over for her.
While I got details on what was going on, and the man’s medical history, from the wife and daughter, I set up the defibrillator; it uses sticky pads instead of paddles, but it’s the same idea. Kit learned in her training to keep going while a second medic works the machine. She leaned out of my way, but still kept pumping on his chest while I stuck on the pads, and then I said to stop while the machine checked to see if a shock was in order: not all heart “stoppage” is the same, and there has to be a “shockable rhythm” for a shock to do any good.
And luckily, we were good to go. We had a chance to save him.
I made sure Kit was not touching the patient; medics have been killed when they got shocked accidentally by a defibrillator. While the defibrillator charged, which takes a few seconds, we both made sure the man’s daughter knew she was to stay clear too. We got her nod. One last check to see we were all safe, and I hit the button.
BAM!
On TV, the person getting shocked does a little jump. In real life, he jumps — a violent convulsion (that is, if he’s lucky: a good muscle convulsion indicates his tissues haven’t started dying from lack of oxygen yet). Our guy nearly came up off the floor. Good!
And …it worked: his heart started again. We got a pulse.
I still had to breathe for him (with a respirator), but after a few minutes he started breathing again on his own.
Kim, the paramedic on duty that night, was on her way in her own vehicle, and the ambulance was still a few minutes behind her. I updated her by radio that we had a pulse and respirations, but I was brief: we still had plenty of work to do; he was far from stable.
Training Pays
Time from pulling into the driveway to shock: just two minutes! That’s teamwork! And I took half a second to think about it. Wow: quick defibrillation does work! He was, as our chief paramedic likes to say, DRT — Dead Right There — and now he was alive, at least for the time being. Then the half second was up (enough celebration! Back to work!)
Another of my First Responder team members arrived and pointed Kim to the correct driveway: she wouldn’t lose those two minutes too.
Kim arrived in the bedroom and got a look at our patient’s heart rhythm. It wasn’t great, but at least he was perfusing (his lungs were getting oxygen to his blood, and his heart was pumping it around). The ambulance was still several minutes away, so we talked about how we were going to get him out of the cramped bedroom, through a narrow hall, and down the narrow stairs.
I was busy enough that I didn’t even notice Kim was setting up an IV while we talked, but when she handed me a constricting band to slap on his arm, I noticed it. 🙂
Drug Route
Immediately a small but firm vein popped up inside his forearm. “Give me an 18 [gauge needle] and I can get that,” I said, and Kim handed me one. I had in it so fast she wasn’t quite ready to hand me the tubing yet. But she got it hooked up and it flowed, and I held it in place while she got the stuff to secure it. We had a secure drug route to help stabilize his heart.
The ambulance had arrived by then, and they actually were able to start getting him ready to go while we finished with the IV. Nice teamwork!
I sprained my right ankle and knee last week, so I knew I wouldn’t be able to help carry the patient, especially since I had spent the last 10 minutes kneeling on the floor. (I was busy enough that I felt no pain — until later….) I started taking stuff out to the various vehicles, such as Kim’s bag, while they moved the still-unconscious patient to the ambulance.
And Now, Another Wait
Because the patient was still critical, Kim wanted an extra medic to go along. Since Kit was actually first in, I called out to her to see if she wanted to go for the ride, but she was inside getting stuff after helping the patient’s dazed wife into the front seat, so I said I could go and we took off.
That’s the start of another 20-minute waiting period: the ride to the hospital. At one point the driver, Steve, slammed on the brakes: a deer in the road. Another hazard of rural areas….
As Kim started pumping in drugs to help stabilize his heart (though the IV), I called ahead to the hospital to tell them what to expect. Things were quiet there at 2:00ish on a Sunday morning. Good.
One thing I like about ambulance work is you spend some critical early time with a patient, and then you get to hand them off to someone else to worry about. When we got to the hospital, there’s another full team to take over: doctors, nurses, a respiratory therapist, and more.
Since I’m not a normal part of the ambulance crew (read: I didn’t have to clean up the ambulance or do the paperwork), I got to watch. It’s darned interesting to watch the E.R. staff work on a critical patient. They had questions about what we did at the house, which I was able to answer, so I wasn’t just a voyeur.
Still Critical
When things calmed down a bit I stepped out to wash my hands, and was back in 2 minutes — and during that time his heart had stopped again. For a second time, one shock brought him back, but Dang! I missed it!
They let the patient’s wife in to see him. When she caught sight of me she was very, very thankful for our quick response and actions. I asked her to call me later to let me know how he is doing. I’ll update this if I hear anything.
(It used to amaze me how many people don’t say thank you. But after awhile I realized it’s OK: they’re often in such emotional shock that they can’t cope with what’s going on, let alone remember little niceties. So when they do acknowledge your efforts, it’s all the more special.)
The ambulance crew finished up the clean-up and the paperwork, and we headed back home. The patient was still critical, and both cardiologists in town were away for the weekend, so the E.R. doc decided to helicopter the patient to a bigger hospital. The chopper crew was wheeling our guy to the roof as we left.
The ambulance dropped me off near home; Kit picked me up and I filled her in on what happened after we left the house. We didn’t get home until 4:30, but Kit and I were keyed up enough to keep talking about it for awhile, and we both finally dozed off just before 5:00 …when the pager went off again.
Luckily, that call was in town, so we didn’t have to go; I reset the pager and went right back to sleep. But Kim, the duty paramedic for the night, would have to go. No sleep for her that night.
What I Hope You Get Out of This
When someone’s heart stops, their only hope is that someone near them knows CPR and starts it quickly — and does it well — until they’re defibrillated, which has to happen pretty quickly too. There are simple units called AEDs — Automated External Defibrillators — that are so easy to use (they literally talk you through what to do) that laymen can use them.
 But it’s better if you’re trained in it first, so take a CPR class that teaches AEDs too. A lot of offices and public spaces have AEDs now. And if you have a family member with a heart condition, considering getting one for your home!
But it’s better if you’re trained in it first, so take a CPR class that teaches AEDs too. A lot of offices and public spaces have AEDs now. And if you have a family member with a heart condition, considering getting one for your home!
But in other places, too. Does, say, your local public swimming pool have one? If not, can you help do a fund-raising drive to get them one? What other high-risk place needs one? Can you help them get one?
Our patient survived because his daughter knew CPR, and because Kit and I were nearby and had a defibrillator. If he didn’t have someone to do CPR and had to wait 25 minutes for the ambulance to arrive, there’s a 100 percent chance he would be dead. Permanently.
Good CPR for 25 minutes before defibrillation? That’s still about a 99.95 percent chance of death. The 9-minute span from my house to his (plus the two minutes wasted by going down the wrong driveway) was probably right on the edge for our patient that night, but he beat the odds.
And that leaves me with proof positive that what Kit and I did made a real difference: we saved his life. Any extra minutes, hours, days, or perhaps even years he has to spend with his wife, his kids, his grandchildren: those are completely due to what we — my whole team — did on Sunday morning.
What You Can Do Now
If you live in a small town or a rural area, I’ll bet your local EMS crews are short-handed, and probably short on equipment, too. Can you help them, with either volunteering yourself or with fundraising? How about good address signs at each driveway? Will a sleepy ambulance crew be able to quickly find every address on your street in the middle of the night? Check your house, your friends’, your neighbors’. Could we easily find their address when seconds count? It all really makes a difference, and sometimes you can make a profound impact with not a lot of effort.
Early treatment isn’t any sort of guarantee: when Michael Jackson collapsed last week, he had a cardiologist in the house with him. He even lived a few minutes from a world-class medical center with top-notch doctors.
Yet he didn’t make it. But even in a rural area, where it’s 20-25 minutes just to get an ambulance to your house, and another 20 minutes after that just to get to a small hospital’s emergency room? Yeah, you can make it even then — if there are properly trained and -equipped people close enough.
My community cares enough that a few years ago we passed a tax increase on ourselves to pay for improved EMS coverage, and that really worked out on Sunday. But it started with the patient’s daughter: she knew CPR, and therefore for a few minutes she was part of my team too. And I’m damned proud to be part of such a community.
You might understand, then, that I was pretty giddy all day on Sunday, which is why I told this story to my email friends, the ones who urged me to tell you the story, too. I’m still a little giddy now, Monday afternoon as I write this. I hope a little of my good feelings rubbed off on you, too, and will help to spread it in one of the ways I’ve suggested. It’ll feel good, even if you’re 50-something …or more.
Patient Update
6 July
I said I’d let you know what happened to the patient if I found out. Very often, even though medics in the field get a heartbeat back, the damage to the heart or brain is too great and the patient dies later, which is why early CPR followed by early defibrillation is so important.
Kit and I were out of town from Monday through Friday, but we stopped by the man’s house this weekend to see if we could find out how he was doing.
His daughter was still there, and she told us that her dad had not only survived, but he was getting out of the hospital today (Monday, 8 days after we took him to the hospital). So it’s a “real” save; he got to leave the hospital and continue on with his life.
Yeah, that giddy feeling is still there for us, but I imagine it’s much, much bigger for him and his family. Kit and I hope to meet him after he has rested up a bit.
(His daughter Becky commented on this post below — jump there.)
11 July
Last night, as I was writing the next entry in this blog, the phone rang. I didn’t recognize the number (which is all I get on my cell phone, which is the only phone in my office), but I answered it because it was local. The caller said his name, and it took me a second to realize who it was: our patient — he wanted to say thanks. I asked if we could come visit him Saturday, and he seemed pleased to agree.
Saturday morning I slept in to catch up on my sleep a bit …and got paged out for a possible heart attack. No, not our CPR patient, but when Kit and I were done with that call, we did go to meet him and see his wife.
They had some questions about what went on that morning, and filled in some details for us, too. He has no brain damage whatever, which confirms his daughter was doing effective CPR, and is chipper, happy, and glad to be able to watch his grandchildren grow up. Honest-to-goodness Good Stuff!
They’re a terrific couple, and it was fabulous to be able to meet him standing up.
Related: A Short Personal Note.
– – –
Bad link? Broken image? Other problem on this page? Use the Help button lower right, and thanks.
This page is an example of my style of “Thought-Provoking Entertainment”. This is True is an email newsletter that uses “weird news” as a vehicle to explore the human condition in an entertaining way. If that sounds good, click here to open a subscribe form.
To really support This is True, you’re invited to sign up for a subscription to the much-expanded “Premium” edition:
Q: Why would I want to pay more than the minimum rate?
A: To support the publication to help it thrive and stay online: this kind of support means less future need for price increases (and smaller increases when they do happen), which enables more people to upgrade. This option was requested by existing Premium subscribers.

I worked as an orderly in my small home-town hospital. There, the job of “orderly” meant doing everything from bedbaths on day shift, to maintenance and security on evenings, and ER on nights. I later rode an ambulance as well; no EMT’s or Paramedics at that time, Advanced First Aid, a bottle of O2, and some air splints was all we really carried.
The feeling you describe, Randy, I felt a couple of times, fortunately. More often, though, it was the sadness that nothing I did, or could have done, helped. The worst thing, as you know now in your home area, is going on calls for friends.
Thanks for sharing your story. My prayers for your patient.
—
Indeed that’s a big change from my previous stint: in a small community, the odds that you’ll know your patient go up exponentially. As you saw, it’s happened to me several times already. It can be gut-wrenching, since it’s harder, and sometimes impossible, to emotionally detach. -rc
The local VFDs (two of them) always have reminders up about having good street numbers posted, visible day or night. Here’s is another good reminder how important that is.
—
Yes, it’s truly a huge problem, especially in rural areas where people are more likely to want to remain anonymous. Works great — but they often haven’t thought about emergency situations. (VFDs = Volunteer Fire Departments) -rc
You earned that good feeling! I work with a couple guys who are both EMTs and volunteer firemen. I have told them before and will again that I’m glad they are around. I haven’t personally needed their skills, but it’s people like them (and you) who save lives every day.
Wow! That’s as much excitement as most people would ever want but is faced by the EMTs all the time! Congratulations! You’re really right about what a defibrillator does. I have an ICD implanted one that’s gone off four times and can attest to its ability to make you jump! Fortunately, the ICD was responding to a spurious signal my heart was suddenly producing. The doctor only kept in from going off a fifth time by moving the contact wire in my heart. It’s apparently almost unknown within the medical profession for this type of anomaly to occur so long as mine after implant. He said, “You’re unique!” Thanks! Meanwhile, you’re truly a Life Saver and a good writer, too!
—
An ICD is an Internal Cardiac Defibrillator — sort of like a pacemaker, but it only fires when it detects v-fib, so someone at risk doesn’t have to wait for someone with an AED to arrive. It runs at a much smaller power because it’s attached directly to the heart (“internal” is the key word!) But yeah, I can imagine it’d really make you jump anyway! Especially when it goes off erroneously, which is indeed rare. -rc
My son just completed 9th grade. As part of the orientation at the beginning of his school year, ALL incoming 9th grade students, the upperclassmen involved in the orientation and many of the faculty became certified in CPR and AED. Parents were also invited to be trained – at no cost to the parents or students. The course was the ECSI CPR and AED training – a two year certification. One quarter of the students in the school were therefore trained to save lives. I believe that they plan to do this every year, so that at least 50% of the student body will always be certified.
—
Cool idea! -rc
Wonderful story. It was almost like a screenplay and even though we knew the ending, it was very suspenseful. That is great writing!
Bravo and big huge THANK YOU to both you and Kit! I’m filled with admiration for what you did that night and for the stand you and Kit take for your community. What a wonderful and inspiring recount of your experience.
One of the groups I support with preparedness education is the Medical Reserve Corps (MRC). I had the great honor of addressing 2,000+ MRC supporters at a conference in Dallas in April — and you are absolutely correct about the great need to support EMT services across the country. I will do my best to share this story far and wide!
WOW! What an eye opener! My hubby has atrial defib, and I think maybe I should learn CPR! Good job, Randy, to you and Kit and Kim and all involved!
—
A-fib is not too serious, especially compared to v-fib, but yeah: I encourage anyone who is commonly around people with cardiac problems to learn CPR — especially if they care about that person. -rc
I have great respect for what your team has done. Furthermore, I am thankful that not only were you able to help the patient and his family, but also that you are in a position to rally the efforts of millions of readers.
As someone who has been on the receiving end of medical aid, I can assure you that the help is sincerely and deeply appreciated. However, I haven’t personally thanked those who have helped me either. It’s not an issue of forgetting “little niceties”; I was in no condition to notice the faces of the people helping me—nevermind get their names. And my family members were in a state of shock too deep to think about anything beyond saving my life. Sometimes the best we can do is “pay it forward.”
SO thank you for everything you do, AND thanks to the other readers for everything they do to make this world a better place!
—
I was in fact referring to family members, rather than unconscious patients, on the “thank you” bit! I certainly understand, and agree “paying it forward” is a great way to do it. -rc
Having spent 25 years as Firefighter/Paramedic, I can remember AEDs being used experimentally around the time the first Life Pak 5 came out and being totally resisted by EMS. This was in the 70s and medics weren’t about to give up any part of running a code. What idiots we were. Well I was glad to see things change and I feel the early defib is the pt’s best chance. Hell, I’ve gone after more than one person with stacked shocks and had him wake up and ask me why I was punching him and then want to get up! Then you got to knock the guy out with versed and intubate him. But more and more are leaving the hospital these days.
One thing about MJ. Did his Doc have any narcan? or any other acls drugs? The people who performed the post did not say anything re. ASHD as a pre-existing cause. Be a shame if he just went into resp arrest due to demerol and the doc did not have any tools.
—
Good question about the narcan, which in Colorado is a BLS drug now. (ALS = Advanced Life Support, typically “paramedic”; BLS = Basic Life Support, typically “EMT”. Narcan reverses the effect of opiates, such as heroin and morphine, which depress breathing.) But I don’t know the answer. -rc
Thanks for the tale, Randy – your friends are right, it *is* nice to hear some good news for a change!
You’ve reminded me that I need to refresh my senior first aid qualification soon – especially relevant, given that, if all goes well, my wife & I will have some new twins around the new year!
As a licensed but no longer practicing registered nurse, I have been saying for quite awhile it is time to get up to speed on CPR again. You have inspired me! Since I also volunteer in the ICU at the local hospital, I see plenty of folks who are in bad shape and sometimes wonder if there were help nearby when they had their accident (or whatever brought them in) that perhaps they would have had a better chance at recovery. Probably not! It was inspiring to read your story and I am so happy for your area that you all are there! Thanks for including it in with the weird stuff !
Great story – hope people take your suggestion to heart. As for me, I’m a teacher in a Senior Center. Tomorrow I will double check for an AED and if there are, if any, trained CPR volunteers and staff.
Thanks for the great share.
—
In a senior center? I would certainly hope so! -rc
Hi Randy et al, having recently spent some time in hospital (due to Pericardial infusion and having a Pericardial window done to prevent a re-occurance), I have seen a number of people who had to be revived after their hearts stopped. The efforts of the Doctors and nursing staff were prodigious in every case. Most of those were saved, but several did not make it. As a 50 something myself (+ 8 !) it does cause you to think about your own mortality. Many years ago, 1970’s, I had occasion to attempt CPR on a lady who had collapsed in the street. Sadly, this was not successful, but never the less, the lady’s husband thanked me for trying. That prompted me to go to classes to try and learn how to do it better, though I have never had the need to use it again (so far!), but we do regularly hear stories of people who have used it, having “learned” it from watching tv programs. Who said tv only teaches violence! These days I am a volunteer on Hospital radio (15 years). My little way of “paying it forward” Keep up the good work with TRUE.
I used to be a volunteer CPR instructor when I was in the Air Force, and I would just like to present my $0.02 for your readers planning to learn CPR. First the public safety announcement: **NEVER Do Chest Compressions or rescue breathing on someone who doesn’t need it!**
That said, find a willing (living) volunteer to “play dead” for you. Take the time to experience what it will feel like to move a real live body around as you try to position them. Have the person let their arms and legs be dead weight as you roll them over. Practice moving a real head around for the head-tilt/chin-lift maneuver and see how hairstyles can mess with positioning.
Most importantly, place your mouth over the mouth of a flesh-and-blood human being. This is not “just like kissing”. There is a visceral reaction that many people have to the feel of warm flesh that they don’t get when practicing on cold plastic dummies. My husband was kind enough to let me practice on him, but I will never forget the shock I felt the first time I had to perform CPR on a stranger. The more you can do to acclimate yourself to the feel of the situation beforehand, the smoother your reaction will be if the time ever comes that you need to use this vital skill.
And thank you to all who work to keep our friends and family alive. Whether we remember to thank you or are too caught up in our emotions to “remember little niceties”, someone will eventually come out of shock long enough to be thankful for your presence at that critical time…. Even if you never get to hear about it, we’re always glad you were there.
We have a vacation home in the mountains. A couple of years ago as part of a fund raiser,our local volunteer fire department “sold” 911 strobes. This is a device that plugs into your phone jack and is linked wirelessly to a strobe light that you mount outside where it can be seen from the road. It activates when you dial 911 to help responders find your house quickly.
If your story get’s one person to get CPR training just think how wonderful that would be. And I would like to personally thank you and all others who take the time to be trained.
As a former Paramedic, your story of this call brought back many memories. Glad to hear things went well – you and Kit and the rest of the team did a GREAT job! Makes me wish I could get back into being a Medic, but a back injury keeps me sidelined……….keep up the good work!
I recently completed First Aid training. Your story is a reminder that I need to get re-certified for CPR, since mine lapsed a couple of years ago. Keep up the fantastic work!
A few add-ons to Randy’s story: your local volunteers are that, volunteers. Whether they are “just drivers” (BS! A good driver gets everyone where they need to be safely & quickly), an EMT, or a medic. All take time & training, from a weekend class to the two years of a full medic. They GIVE that time to their community. No parades, no pictures (press up at 02:00? On scene before Randy & team are gone? Not hardly), sometimes a thanks, and the self-knowledge that they just positively impacted a whole lotta lives that few will ever know about.
Second: if you want a CPR/first aid class, contact your local EMS squad, often they offer the classes for free or at a substantially reduced cost.
Be safe out there.
Two comments:
1) Our rural county in Virginia has a requirement that all homes have a number sign at the driveway. These high visibility signs, blue with white lettering, are custom made and sold by the volunteer fire departments for $10.00. Compliance is about 90%. It makes it easy for fire and rescue squads to find the right house day or night.
2) A service organization, Ruritans, to which I belong, places easy-to-use defibrillators in strategic locations in the county — churches, schools, public facilities. These defibrillators are designed to be used by persons completely unfamiliar with their use, and are equipped with step-by-step spoken directions for their use.
When I was a police officer in Florida, I started a movement to get an ordinance passed to require all homes/driveways to be marked with an address. My adopted community of Union County, GA. has started a huge effort to readdress all roads, etc. in the county using a system designed to help first responders, even non-residents, find a location in an emergency.
—
We have found resistance to that in our community. People don’t want their addresses changed, no matter what the rationale. We have side streets with the same name as the main road, some random addresses (instead of orderly progression), a mix of odd and even numbers on the same side of the street, etc. It’s a nightmare, and actually fairly expensive (in paid workhours) to fix. We’re slowly making progress, but it causes delays in the meantime. I fear we’ll have to have a spectacular failure (such as the death of a child) to get people to pay attention to the issue. -rc
I worked in state institutions for over 25 years and know about emergency response. The State of MN has the blue and white address signs on every driveway. Our tax dollars at work for the common good.
—
It’s a good investment: it actually saves money as well as helps save lives. -rc
Another Standing Ovation in front of my computer screen.
To give a different perspective, here in Japan everybody does CPR training (admittedly only one hour) when getting a driving license, on the grounds that you may be the first person to arrive at an accident scene.
I have never had to use it, but one week ago today I arrived home from work, and as I was fumbling for my keys to open the front door, I hear a sound like a bicycle falling over, followed by a few shouts that made me walk/run around the corner to see what had happened.
For the next few minutes I found myself standing over a young man who had been run over, reassuring him that the ambulance would arrive soon and reminding him that under no circumstances should he move, while two others directed traffic around him.
Since that was the entire extent of what I could do to help him, I felt pretty useless, but at least I think I did better than the half a dozen people who stood at the side of the road watching, (eventually a couple of people came out to talk to him and hold an umbrella over him since it was raining), and definitely better than the bastard who hit him, who apparently did not deem it necessary to stop.
On an aside, Japan has recently started putting AEDs in public places in the same kind of “break glass in an emergency” boxes as fire extinguishers, which is a good thing.
As regards MJ, one thing bugs me. The recording of the 911 tape had the following (paraphrased) interaction;
Caller: We’re giving him CPR on the bed”
Operator: “You have to move him to the floor”
One thing they taught us in that one hour course was that CPR is ineffective unless you have a hard surface underneath the patient, as it does not compress the chest cavity. Surely the doctor who was present should have known this? Or is my understanding incomplete?
—
Any doctor should know that, let alone a cardiologist (which MJ’s doctor is, according to press reports). And don’t minimize your participation in the hit and run: talking with the injured patient is very important, as is standing over him to ensure he doesn’t get hit again. You did good! -rc
In rural Carmel Valley, CA, the volunteer fire department would deliver presents to children (their parents dropped the presents off at the fire station beforehand)–one guy got to dress as Santa Claus–which gave them practice finding addresses that were unmarked or down long driveways. They would look around at the addresses on the way to the lucky recipient’s house as well. This project also reminded folk that we had a VOLUNTEER fire department, and of the importance of supporting the firefighter volunteers, besides offering the firefighters a big chunk of holiday fun showing up as Santa to all those little kids. It was a great idea.
Once again, thank you for sharing your experience, strength, and hope and touching people that you will never know! Having grown up in a small farming community with a VFD, we were taught early about emergency first aid, but also respect and appreciation for the volunteers. Thank you, thank you, thank you to both you and Kim for your efforts on behalf of your neighbors and friends.
In addition to addresses so that emergency responders can find locations, I’d like to give a mention to the Vial of Life project (google “vial of life” for more information). This, too, can be a lifesaving tool . . . and it is free. Mine is taped inside the door of my refrigerator with a magnet on the outside letting emergency responders know where vital medical information is located.
Thank you for sharing the story with us (and to your email friends who encouraged you to pass it on). A story appropriate to your “Heroic Stories” eletter! 😉
—
Just to clarify, I have had nothing to do with the HeroicStories publication since 2003. -rc
I turned 50… on Monday! Not a good time to get the “I’m getting older” feeling as high-profile people your age are dying and you’re thinking…”I wonder how MY heart is, though I’ve never had any problems or indication of problems…?”
I do really appreciate your service and especially your sharing about it. We have a special needs child and have “had to” work with a few EMT’s (volunteer and paid) in our time. It’s great to hear first hand about your end of the experiences that you are a part of. Thank you to ALL the volunteer EMT’s who so selflessly help others in need!
Now – I think I’ll go do some cardio… 🙂
Thanks for the inspiring story, Randy. Makes me nostalgic for the days when I volunteered at Broomfield Ambulance in Colorado. At the time, it was a fairly quiet community, but being so near to a major highway, we got our fair share of harrowing episodes, as well. I agree, it’s a truly good feeling to know that you’ve helped someone, no matter how small or large that contribution was. Keep up the good work, and kudos to you and Kit!
Great story Randy. Congratulations on the save and thanks for your commitment to your community. There is a large semi-rural area outside the city here with many unmarked driveways and even unmarked roads. There was an effort some years ago that coordinated with a local sign company to encourage folks to get reflective address signs for their houses or driveways to speed the emergency response times. Of course that makes it easier for friends to find them too.
Your stories make me miss my days as an EMT.
As for the Michael Jackson CPR situation – I heard that the doctor said he had placed one hand under MJ’s back when he started CPR. That’s means he was only doing one handed CPR on an adult on a bed since a hand wouldn’t be a hard enough surface to press against. Basically useless. Since he did have a weak pulse when first found, I wonder if correct CPR had been started immediately, and continued until the ambulance arrived, if MJ might have survived.
Inspiring story, Randy. Kudos to you and your team for recognizing a need and stepping up to the plate to fill it.
I recently received my CPR/AED/First aid certification and also started working for my local Red Cross chapter. When I read your story, it reminded me of one of our mini “missions” – to have at least one CPR certified person in every home.
So additional kudos to the man’s daughter who will have a sweet tale to share with her grandkids when she’s old and gray. BTW, if by chance, she was certified thru the Red Cross, she may be eligible for our national “Heroes” award.
Thanks for posting the story. I actually started a first aid course today (two day one, covers everything from burns, CPR (including the defib) to heart attacks), although it wasn’t quite inspired by your post (I had booked it last Friday). But your story really has inspired me to actually go out and do something more, like actually volunteer at the red cross or start giving blood.
Thanks for that.
—
And thank you! -rc
In our rural area we offer reflective address markers at a very reasonable cost and try to encourage people to purchase one. It really makes a difference, especially in the middle of the night. It’s also worth noting that the problem of locating addresses is not limited to rural areas. Many times it can be just as difficult in the city!
I hate to say it, but sometimes living in a city with a well staffed EMS/Fire department does not always mean you will get a quick response.
A few months ago my future mother-in-law had a bad attack of A-Fib, and we had to call for an ambulance to get her to the ER. The driver had trouble finding the road we are on, even though it has all the signs. Thankfully, she did not need any lifesaving care, but it still scared me to hear the driver commenting randomly “oh, I never knew this road existed.”
—
I used to drive an ambulance in San Francisco. Every day I went to a street I had never heard of before. That’s what maps are for. And in fact, the call I wrote about here was on a road I couldn’t have told you where it was based just on its name, and I had never been on it before. Dispatch told us the cross street, which headed us the right direction, and the map told us the rest. It’s not rocket science…. -rc
A great story. I’m teaching CPR in 2 weeks and I would like to use your call to reinforce the usefulness of timely AED intervention.
—
Feel free to tell them the story, and/or give them the URL to get “the whole thing.” -rc
I have had the good fortune not to need the CPR training I have had for 31 years now. A few years ago AED’s were installed in our workplace. Since I work around High Voltage equipment, my employer offers CPR training on a recurring basis; but, since we had AEDs, the outside trainers wanted to omit the classic CPR training. I raised cain citing that something like 80% of our lives are spent away from the AEDs. The company safety specialist hosting the training session agreed with me, and we got the classic training as well.
Oh, and let me pass along an anecdote about “not stopping.” My predecessor in the broadcast engineering business had a heart attack many miles from any medical assistance. His wife threw him in the back of their station wagon and drove like crazy. He was later heard to say “I thought she was going to kill me;” since every time she hit a bump in the rural road, his heart would “hurt like hell” as it beat once or twice in response to the pounding. CPR may not have any obvious effect, but it may be “just enough.”
—
As you realized, you cannot depend on the AED to do it all; CPR is also necessary. And, in fact, the AED will say “Start CPR” quite a bit. Seeing how actors do it on TV isn’t enough, since they’re faking it. You need to do it on a dummy to understand how hard to push, and you need someone who is trained to be a trainer to correct you when you’re not doing it quite right (most do it too shallow, and too slowly). There’s just no substitute for actual training. There is also nothing like doing it on a real person to really get it. Trust me on that: I’ve done it on many dozens of real people. -rc
Why don’t ambulances use the “NEW” GPS devices? Supposedly you can put in an address and it tells you where to turn?? I’ve never used one, just wondering If they are used.
—
Many do, but the crew has to know what areas they’re weak in, because the quality depends entirely on how accurate area maps are. And in our area, the maps aren’t just “poor”, they suck. Example: to get from the house in this story to the hospital, it tells you to turn on a road that doesn’t even connect to mine. It “thinks” it does, but it doesn’t. It’s so bad that they actually slow you down if you’re not careful by causing wrong turns. -rc
I am a first responder. I have used the AED twice, the first was a ‘save’ a 16 YO who had taken some of his fathers RX meds (given BY HIS FATHER). It was the first save in the county after we received AEDs. All of my children know CPR from going to the classes with my husband and myself (they can’t be certified in the same way I am) but have used some of the skills learned while attending classes with us. They have been attending these since they were very young and now between the ages of 14 and 26. Children are capable of learning basic first aid and CPR. Use your best judgment regarding your own child’s development and abilities.
One day when my daughter was a baby, she got something in her mouth and started choking on it. My wife got there first, but panicked because she didn’t know what to do. I took the baby from her, and got the item out of her mouth, using what I had recalled from various training I had gotten as a teenager. She signed us up for “Infant CPR” the next day and we both got trained, in case it happened again (it didn’t).
New parents – don’t wait. Get trained. The first one on the scene is YOU.
—
Hear hear. That should be completed before birth. -rc
My employer has offered CPR classes for several years and has installed public-access AEDs throughout our properties nation-wide. Fortunately, as a first responder, I’ve never had to perform CPR. When the day does come, though, I’ll be able to utilize my training. The machines are of such value that I’ve been kicking around buying one to have at home.
Good work on the save. I had a “fatal” heart attack four years ago, and I’m here to read your story because of an EMT just like you. I did go back to thank him after I was released from the hospital, and he was delighted. I wish and hope more people will say thanks to the EMTs that are there to help no matter how gawdawful the hour or circumstance.
—
I loved it on the extremely rare occasions patients sought me out to say “what happened”. Don’t be afraid to do it, even if it’s been awhile. We would like to know! -rc
God bless you, Randy, and all the volunteer EMS personnel who wear those pagers. I work now at the other end of that ambulance ride, and I am the guy at the head of the ER cart when you folks roll in, standing amidst a million dollars worth of monitors, drugs, scopes and lots of other stuff. Having worked at the other end of this evacuation chain for many years, I still marvel at the dedication and professionalism of the volunteer caregivers out there in the communities. It’s been said before but bears repeating: good first responder or bystander CPR, and early defibrillation make a world of difference.
Trauma calls, too — securing the scene and the patient’s safety, opening the airway, controlling bleeding and stabilizing spinal injuries — point up the importance of educated EMS folks out at the pointy end of the spear.
Kudos to you and your teams. Keep up the great work.
Very interesting and well-written story, Randy. Congratulations to you and Kit.
I was a police officer in Tucson, Arizona, for 22 years. In the 1970’s, we were offered EMT-II certification which I took. At the time, it was one step below Paramedic (which was just getting started in Tucson) which was within the Fire Department’s program.
I was given — and still have — a “Laerdal Pocket Mask” in a hard plastic case. This is a soft plastic mask that fits over mouth and nose with a one-way valve to prevent aspiration of any exhaled breaths into the rescuer’s mouth. The case contains easy to follow directions for use. This is useful (as commented by an earlier writer) to help avoid the “weird” feeling of direct mouth-to-mouth contact, and also help prevent the spread of body fluids from potential AIDS patients. Laerdal still sells these masks for $9 to $12, depending whether you want it in a poly bag or a hard plastic case. I keep mine in my truck glove compartment where it is handy all the time.
Thanks for all you do.
—
You’re not likely to get AIDS from saliva, but there are plenty of nasty things you definitely could get, so such a mask is smart to have. -rc
Many of us have been trained in CPR but over the years we forget the timing. Do you think on one of your news letters you could remind us how many chest compressions before we tilt head and sweep mouth. Then how many breaths before we go back to chest compressions. It seems like we will always remember the technique but not remembering how many times for each procedure is what makes us nervous. I can and will look it up on the net but thought this may help others. Also thank you, Your Wife and your team for being one of the good guys that dedicates your lives to helping others.
—
It’s now 30 compressions to 2 breaths, but the most important thing is a fast and reasonably deep compression. You may remember 5 to 1, but studies showed it took 2-4 compressions to prime the heart with enough blood to really get it pumping, so 5 really isn’t enough. And how fast is fast? I covered that in one of my videos! 🙂 -rc
THANK YOU for sharing this story with us!! I held my CPR, First Aid and Lifeguard certifications for years but they lapsed several years ago and I never quite got around to re-certifying. Your story has really motivated me to get those certifications back now. And a hearty GOOD JOB to you as well!!
Randy, people like you and your team give me hope for this country. God bless y’all.
—
If you want to change the world a bit, you can’t just complain about it, you have to do it. Simple as that! -rc
You Americans are lucky. Here in England main roads have very few name signs. While holidaying in one of the Channel Islands, we commented on the almost complete lack of road name signs. Our taxi driver’s reply was “We locals know where we are. We don’t need signs”.
It is wonderful that there are people like you and all of the others are trained to do EMT work. It’s more than giving, way past that.
Great job guys. I lost both of my parents to heart attacks. I didn’t know CPR when my Dad died so I learned it, couldn’t have helped there because I wasn’t home but, the hope is that if ever it’s needed I know how. Secondly my mother died away from home by herself so no one could help her either.
But you can bet everyone you’ve helped if asked later, they would sell the farm for ya.
Bravo. I’ve never had to use much of my first aid/CPR/self-aid training – but I certainly stay current. One thing another reader mentioned was infant CPR. As a parent of three, I’ve been lax and am being recertified. I’m once again inspired thanks to the story.
I also believe readers should be aware there (used to be) three different types of CPR dependent upon the victim’s age. Obviously, an infant doesn’t need the same compressions or breaths as an adult, but neither do children until they’re almost teenagers. I’ve always believed the differences are important. Why not teach those differences in all CPR classes, even if it’s information only?
As before, keep it up, Mr. Cassingham. And the Mrs. as well!
Congratulations! As a retired paramedic of 22 years beginning in 1972 through 1994, I applaud your efforts. A good portion of my years were as a volunteer in West Virginia and we have our share of rural spaces. I moved up the food chain to paid staff, flight medic, management. Those are other stories. Suffice it to say, AED’s and CPR are lifesavers but good people, willing to volunteer are just as important.
KUDOS!
It is always nice to read a nice heart touching story. My daughters have a seizure disorder so I have always been CPR and first aid certified but I was surprised to learn that most classes don’t teach you seizure training so I always try to tell people if you are going to train go the extra mile and get seizure trained as well; you never know when it may be needed.
I read your ‘This is True” column every week, usually while shaking my head at the stupidity.
This story was inspirational. Well done to both of you for being the people you are and for what you are able to do to help other people. It’s people like you who give me hope for the whole of mankind. Thank you for publishing the story.
Thanks for the story, I always like to hear when we in EMS actually do make a difference.
But it is the first First Responder who saved that guy, his daughter. You are right, CPR and AED are extremely important to saving the lives of cardiac arrest patients, and that is why I’m a CPR-AED Instructor as well as an EMT. Defibrillation only works if the tissues are viable, and the daughter kept them that way long enough for you to arrive.
Congratulations on the save. They are far too few times that we get the patient to the hospital alive, and even fewer times that the patient goes home that way.
In Queensland, Australia where I live they have implemented a rural numbering system to save lives in emergencies like you mention – as well as being darned convenient.
Each property has a steel star picket at its driveway with a cover on the top with reflective numbers stuck on. The numbering system is based on distance from a road intersection or other landmark in metres divided by ten.
It is so handy if you are at 689 & looking for 789 you know it is a kilometer ahead. Slight variations occur because of driveways close together but that’s basicly it.
A great idea was that the councils gave the contracts for installing them to community groups like the Lions etc to install them so it gave them an extra income & installing only required a person with a car & star picket driver.
Before this was implemented, our road had about 8 Lot 2’s because of subdividing over the years. If a marker is damaged or stolen then a new one is fitted free of charge by the council.
There’s a special place in heaven for you and your team, and all your brethren in arms. The Talmud says that a person who saves just one life is as if he had saved the world.
As a memorial to my parents, I purchased a defib for the synagogue they attended, for years, before they moved away. (My older brother in Baltimore, where my parents had moved, in their 80’s, had done this, so the idea wasn’t mine.) This required several members of the congregation to take classes in its use, etc.; and, shortly thereafter, a congregant who was choking was saved by a member who had learned Heimlich in that class! Every house of worship — especially one where “we older folks” attend, should have one, and people trained to use it. Same old story: better to have it and not need it than to need it and not have it.
Thanks for this story. I learned paramedic while doing my civil service (instead of joining the army), and so far, I had to do CPR only on dummies. Thanks God I never had to do it for real, but on the other hand, I’m sure I could do it. (I don’t work as a paramedic, I’m a computer geek.)
You are right, there have to be lots of people knowing CPR and First Responders are a very good thing. Here in Germany, often people tend to think it isn’t their responsibility, it should be something the professionals should attend. They are wrong.
Thank you also to Brian from Australia. The system you’ve got seems like a very good one, especially in the not-so-crowded regions of outback Australia. I’ve been there in 1992, and I liked it very much.
To everybody else: learn CPR, support First-Responder teams and every professional paramedic. Look that your address is easily findable. In most towns in Germany, that’s easy, but there are also towns in rural areas where the house numbers are given by the time they were built, so it’s hard for any outsider to know where number 319 is…
A local high school lost a 15 year old during a basketball game a few years ago. His parents started a fund to supply defib machines to all nearby schools. The drive was so successful that not only do ALL the local schools have them, but now they are available at local malls, shopping centers and libraries. They’ve been put to good use a few times already…to great success.
Congrats on a good save! They don’t like to tell you the actual odds of success in a layman’s CPR class, for fear of discouraging people from trying. What the scaredy-cats don’t recognize is that when the odds are between “slim” and “none”, slim still beats none. It’s worth trying. I’m re-certifying at the end of the month, myself. Like Volker, I’ve only had to do CPR on dummies, and like him I’m grateful for that. Still, it’s something that everybody should know.
As a former Army Combat Medical Specialist, I understand completely. That is awesome what you and your wife do. Keep up the great work! It’s great to know that there are others out there that care for more than just themselves. You guys are awesome!
When I was in the army, they instituted their version of the first responders (which was instigated by my medical platoon) by training solders with advanced medical training so that they could help us on the battlefield by performing life saving techniques on their buddies until we could get there to do the heavy work and prep them for evac to the rear. I think the same is important in the civilian world. In cities and suburbs, EMS is here almost before you hang up the phone, but in rural areas, as you pointed out…it could take some time. I think everyone should learn how to at least do CPR. When someone’s heart stops…seconds count. Having someone there immediately doing CPR can mean the difference between life and death.
Yeah Bro! Nothing like that rush, and the Talmud is right.
When my family and I moved to a small town on Long Island 13 years ago from NYC, I looked forward to becoming a firefighter, specifically a first response medical crew. One doesn’t get that chance in the big city. I’ve got 5 kids and when we hit 60 stitches in one month, I decided it was time to get more serious training. I’m also a scout leader and teach the boys maybe more than a basic first aid. Thank you for your article. We can’t impress the importance of being CPR certified too strongly. If you get a group of 7-10 people together, my department will come out and train you. I think most other volunteer fire and ambulance companies would. Ask yours if you are not a member.
I teach my children and my scouts that one has an obligation to give back to the community that nurtures you. At 53, I’m too old to go running into burning buildings though many of my company would disagree for themselves but I can handle an ambulance and memorized all the street locations in our town.
After 911 we had a major influx of new members which has now dropped off. All volunteer companies need members. Even if you only sweep the truck room, its important in getting the ambulance out. Good luck to all first responders.
Timely story for me as I am due to turn the big 5-0 on Friday, November 13 of all days, if you are superstitious.
I have kept myself certified in First Aid for the past 20 years. Started as a job requirement – Early Childhood Professional – but continued as a desire to be update and able to help if needed. Here in Canada you are excepted to re-cert in First Aid every 3 years and, if possible, every year in CPR.
I have used my training to help two choking victims. An infant Mom had given popcorn to was projectile vomiting. Nature had solved the problem but I was able to educate the Mom on not feeding popcorn to the infant anymore.
Then a co-worker at lunch one day was talking and eating and next thing we knew choking. Coughing did not dislodge so Heimlich was applied and then I insisted she get checked out as I had learned at my latest re-cert (weeks before) that Heimlich could injury you internally sometimes. Good thing I insisted, she is a tiny 90 lb soaking wet thing and it turned out she was just recently pregnant with her second child, she was fine but at least we knew for sure.
As you say, it IS difficult to find a particular driveway in a rural area. It would be far easier if everyone in a rural area had their own reflector code since finding reflectors at night would be much easier. No two reflector codes can be the same. Drive up and down the road to make sure. Mount them on your mail box. Let’s say white over white over red. Or whatever. Get everyone in your town to do it.
—
Codes don’t help when you’re looking for an address, and an address is what “enhanced 911” gives the dispatcher. Don’t make up a code when all you have to do is buy reflective numbers and put them on a reflective sign! $10-15 will do it. -rc
Thank you so much for what you do. I’ve had to call paramedics to my house a number of times due to my partner’s heart and diabetes complications. I’m always amazed at how you emergency workers can stay so composed in the midst of a crisis. I can’t thank you enough for being there when we need it the most. What you do is truly valiant and generous.
Congratulations on a SAVE … I know the outcome isn’t often very good, and he still has a long way to go before he’s fully recovered. I’ve had cops tell me that 25 minutes of doing CPR by yourself while waiting for the ambulance is the longest 25 minutes of your life.
I was a volunteer EMT in Granby CT many years ago (I’ve been in Oregon for 20 years) and know how dedicated you need to be to do the best for your patients. Granby is about 35 square miles and is still a fairly rural town, although it has bedroom community pockets. We also covered East Hartland, to our west, and some of our coverage area was almost an hour from the nearest hospital … although when Hartford Hospital put their helicopter on line it brought them much closer. We were a “scramble” unit … meaning that we had pagers or were near a phone and responded to pick up the ambulance enroute to a call (which added to response times). The police were our first responders, because they were already on the road, and we had everything from cops with minimal first aid training to some of the ambulance squads best EMTs. In fact one of the best is now the police chief, and I’d trust him with my life in _any_ capacity.
Connecticut at that time had their own training curriculum and did not recognize National Registry, but they now follow the National Registry curriculum. I was one of eight in our squad who took another 100 hours of advanced training to what Connecticut at that time called EMT-I (on top of the EMT-BLS), which gave us three appliances … EOA, MAST and basic IV therapy (lactated Ringers and D5W – no drugs). EMT-D was another training level that could be added to BLS for defibrillator.
For a while the Canton Ambulance had _two_ EMT-Is, a husband and wife, and at least one of them was available in town 24 hours a day, 7 days a week. That is way too much to expect from two people.
I recently was told by someone who is still in the squad that Granby is considering going to full paramedic level … a HUGE commitment for a volunteer unit.
Hartford Hospital’s helicopter can reach any place in the state within 12 minutes from liftoff. ANY EMS certified person can call for the helicopter, if they feel it is needed. They had expected an inappropriate call rate of about 15% until EMTs were used to the protocols but after 6 months in service, the hospitals helicopter staff told us that they had _never_ had a call that they felt was inappropriate. There were some in which they assisted to get the patient into a ground ambulance, rather than transporting in the helicopter, but they said that even those calls had not been inappropriate.
Living in a city now, with the fire department paramedics responding within minutes (during the day they hang out at the community center gym … 2 blocks away), as well as ambulance medics, we’re not very far from trained help if we need them. But, as in Colorado, there’s a lot of open country not very far from the city where an ambulance can be a _long_ way away. Having had my last training over 20 years ago, I really don’t feel a lot of confidence that it would all come back to me if I stopped to render care at an accident miles from trained help.
I keep thinking that I really should at least renew my CPR certification. Maybe your success will inspire me.
Perhaps this makes no practical sense since most of us would not be able to distinguish between ventricular fibrillation, ventricular tachycardia or bradycardia, or no cardiac rhythm at all (“asystole”), but given that Automated External Defibrillators (I have read that the Philips model is the only one approved by the FDA for use without a prescription and specific training) seem to begin at around US $1,250.00, meaning they are beyond the financial reach of many farms, homes or apartments, is there information on how to rig a MacGyver-type defibrillator from such things as extension cords? Since I realize that such information might violate all kinds of medical/professional or even legal guidelines I certainly wouldn’t expect or ask for you or any of your readers to get into jeopardy, nor would I want to create further risk for a person who has experienced a “heart attack” or those around them. Still, when minutes are critical, I have to wonder if there isn’t something that the American Heart Association and other medical professionals would have recommended or done (in addition to CPR) before there were AED’s on the market?
—
I’ve seen a couple of such things on TV, and I rolled my eyes both times. There is no way to give the right level of current for the right amount of time with an extension cord, period. Don’t even think of trying it. Odds are much higher you’ll kill a healthy person doing that than help an ill person, so it isn’t even worth thinking about. -rc
Thanks for all you do, both with True AND with being a real-life hero. After reading this, I immediately looked outside to be sure that I can see my neighbors’ house numbers. They all have numbers, but I’m sure mine are too small. Now I’ll make a change!
Step-by-step “spoken” directions for their use may not help the 8% of the population with hearing impairments.
Aren’t there new methods being suggested for CPR that recommend using only rapid chest compressions and not the mouth to mouth, as there is enough O2 in the blood to enable the brain to survive?
Of course, I understand that specific training in this method is recommended.
—
Yes, there is an issue with “talking” AEDs for people with hearing impairments. Lay CPR training does emphasize compressions over breaths, but that will only work for so long. -rc
I had chills running up my arms by the 2nd paragraph after “SUNDAY” and a watery eye by “DRT” — as a fellow 50 “something” I’m glad your 50-something email friend convinced you to share this story.
Kudos for all you’ve done and accomplished.
As a General Surgeon with many days of E.R. experience and a year in Viet Nam, I have saved several lives – the experience NEVER gets old. I know just how you feel.
You’re right, the MacGyver trick would almost never work. It’s not just the amount of current. Timing is also super critical. A shock during the wrong time in the cardiac cycle can actually cause the heart to fibrillate. Also the current should be direct, not AC.
Incidentally, the 60 cps that Tesla chose is the most lethal cps possible because it is so close to the timing of the normal cardiac cycle. This is one of the reasons that electrical shock is so dangerous. No one knew that at the time, and changing it now would be impossible.
One thing that seems never to be emphasised enough is that you really have to compress the chest, with 100lbs/44kg pressure, so small people are at a disadvantage.
I’ve always thought that compression by foot would be more effective (less tiring, more pressure, wider area to avoid broken ribs) than the heel of the hand, especially if you only weigh 100 lbs. But for the breathing, you would need a 2nd person.
—
The amount of pressure needed isn’t constant at all: depends on the size (etc.) of the victim. A foot might work, but would be much harder for most people to get a controlled compression. -rc
Here’s a paper about a new CPR method that might be the one that Bob heard about:
Rhythmic abdominal compression CPR ventilates without supplemental breaths and provides effective blood circulation. (National Institutes of Health site)
“CONCLUSIONS: OAC-CPR generated ventilatory volumes significantly greater than the dead space and produced equivalent, or larger, CPP than with chest compressions. Thus, OAC-CPR ventilates a subject, eliminating the need for mouth-to-mouth breathing, and effectively circulates blood during VF without breaking ribs. Furthermore, this technique is simple to perform, can be administered by a single rescuer, and should reduce bystander reluctance to administer CPR.”
—
In English, the study showed that doing abdominal compressions not only squeezed the heart, but helped move air. The study was done on pigs, not humans. Bottom line: things change all the time as studies are done, which is one of the many reasons one needs to recertify frequently, and follow what you’ve learned in your latest class. Doing “experimental” procedures could result in lawsuits. -rc
8 years ago, I survived eight hours of supra ventricular tachycardia. My heartbeat was 195-198 bpm and I thought I wasn’t in trouble, because my mother’s implanted defribrillator doesn’t ‘go off’ until her heart reaches 200 bpm. After eight hours, I called her and asked her what to do! She later said she had a really hard time NOT crawling through the phone line to get to me, but to say as calmly as she could that I needed to be seen as soon as possible.
By the time I got to the outpatient clinic I was so weak I fell down after opening the door! They got the ECG while the ambulance arrived to take me around to the E.R., a couple of blocks away. I hadn’t realized that my mother meant EMERGENCY ROOM, not just be seen by a doctor. 🙂
The damage is permanent. My activities are even more limited than they were 18 years ago when I had to leave WSU with CFS/Fibromyalgia symptoms. But I lived to enjoy your sites. Thank you for continuing with these great sites.
As a former paramedic and now a certified general surgeon and specialist in emergency medicine, I’d like to give a tip how to keep up a rhythm of 100 compressions per minute while doing cpr: Sing to yourself that AC/DC-Song “I’m on a highway to hell…” and you got the right rhythm. But: Do it silently when someone else is around!
—
My 20th video dealt with this very subject. -rc
My wife and I have taken CPR classes through the Boy Scouts of America. We have four kids with the two older boys being in scouts. The training is annually and classes are given to the boys and adults. The classes are part of the boys merit badge for first aid and last for several weeks. They have to complete hands on test along with book work. We always hope that if the time should come that any of the boys or adults would be able to respond. I’ve had friends saved by EMT’s in the past and even in the moment or after I never thought that, “Thank You” quite covered the emotions that I was trying to express.
I experienced a mixture of chills, thrills, and near-tears reading your recounting of your “adventure”. I was a volunteer firefighter and EMT for several years and only had to use the AED that we carried on our rigs once in real life (can’t count the number of times I had to go through the protocol in training), so I know what you are feeling. It is good to be able to save a life when you deal with so much death and suffering.
The only experience that is more profound than saving a life is helping to bring one into the world (yes, I got to assist in a pre-hospital birth).
—
I did that once too, but it was so fast that I hardly got a chance to think about it. -rc
That is what being in medicine is all about. Having spent the last 20+ years of my adult life in ER medicine as a PA I have slogged my way through a million sprained ankles, sore throats and runny noses but about once or twice a year you really SAVE someone’s ass!!! Take that memory, bronze it, cherish it, relive it and re-tell the story. That is what will get you through the nights of multiple calls from drunks that got a boxers fracture from beating up their spouses, drug addicts that desperately need a fix (and decided that EMS was the best place to get one) and runny noses that need some nasal spray but the patient couldn’t afford the cost (despite the $5.00 pack of smokes in their pocket.) Ya it’s a great feeling, hold on to it for as long as you can.
—
It’s one of the reasons I decided to write it all down when it was all fresh in my mind. 🙂 -rc
I am a former EMT and wonder how Michael Jackson’s doctor did not seem to know that CPR does not work well when performed on a bed.
—
Doctors aren’t usually very well practiced at in-the-field emergencies. On the other hand, this guy is supposed to be a cardiologist. It will be interesting when the “real facts” come out later so we know what really happened. -rc
AS a retired EMS Liet. for the FDNY with 33 years as an EMT, your story had me on the edge of my seat. Since retiring, my two jobs are as an EMT with the local EMS service in my rural PA town, and as an AHA CPR instructor. Your description of finding a rural address is so true. We get addresses like “turn left on Rt 715 and look for a blue house next to a big rock.” Also keep pounding the drum about getting CPR & AED training. As you just experienced, trained, caring people with the right equipment can make a difference. Congrats to you & your team on a good save.
Loved your article. Live in a city and had a cardiac arrest a few years ago. When I started to fill unwell, I used my mobile to call an ambulance. Apparently an off-duty nurse came over to my parked car to help, and I was rushed off to hospital. I immediately had surgery, survived and am doing well. Never thought much about it, really, I was in my fifties and and felt satisfied with having lived my life. However, your article is a wonderful account from the side of the medics who are involved in the drama of it all and who bear a responsibility to a total stranger. In a city one does not know the people who have helped me survive – so I am using this opportunity to say “thank you” to those who help others with their skill and knowledge. I have enjoyed my years since and have lived with much joy to see a new grandchild. Thank you from me to all of you – for those of us who never get an opportunity to say thanks to the individuals.
I’m currently a volunteer firefighter, and a former member of a First Response team. I know all too well how quickly a story like this can turn to tragedy. Randy, I’m so relieved that you got to experience a positively uplifting call. I went through a similar call several years ago, and I still remember the wife coming to the station a week and a half later and thanking us for saving her best friend in the world, who she would be forever lost without. Money can’t buy the kind of feelings you get from doing that for somebody.
Having run two military ER’s, I know first hand how critical time is in this situation. Bravo, a job well done. But also a caution: it don’t happen this way often…because of the time element. Savor the feeling for as long as you can, and remember it the next time one of your patients doesn’t make it.
I’ve always thought about getting my CPR license. I think because of your story and what my father recently went through with staph in his spine…a moment’s notice that everything in your life can change, that changes everything. After Ike, my dad got really sick and we took him to Veterans Memorial where they overdosed him on morphine 3 times and we almost lost him. They didn’t know what was wrong with him. He was out of his mind. Sometimes it was funny, others not so much. He was talking about them killing him and where we would bury him. Finally, out of ICU..when they stopped feeding him Morphine…and Penicillin which he’s allergic to…they told him he’d never walk again and down to the Spinal cord injury unit….He’d been bed-ridden for months…finally, they found what was wrong and he was coming around…staph in his spinal cord…I’m glad to say that he started walking slowly…Christmas…and He’s now fully…well, mostly recovered…that alone is enough to make me want to be able to protect my family more and be a certified CPR person. Thanks for the story! Things like that is what make you realize that we take life for granted way too much…
When I was President of my Jaycee chapter, years ago, we sponsored a CPR course. Less than twenty four hours after the final session ended, one of the Jaycees in the course was driving with his family when the car in front of him started driving erratically and left the road. Sure enough, the driver had had a heart attack and died at the wheel. The Jaycee was able to pull him out of the car, perform CPR for about 8-10 minutes until an ambulance arrived. The guy made it. I had that giddy feeling you talk about and all I did was schedule the course!
—
Sweet! -rc
Your local Red Cross often offers CPR/AED classes. They last all day, usually, and once certified, you can go back annually for recertification. There is a modest fee, but it’s well worth it.
As a full-time 911 Paramedic and the 1st Lieutenant of the Desoto Rescue Squad when I am home I wanted to say two things:
1. Congratulations on your Save! Good Work, you, Kit, and the rest of the team should be proud!
2. I appreciate you encouraging folks to volunteer their time, I know our Squad is undermanned and are always looking for good folks who want to make a difference.
—
Individuals can make a difference …but only if they go out and do it. -rc
Congrats Randy and Kit – and the whole team from first responder all the way through to the hospital. I’ve been in EMS for 25 years now, and I’ve long since hung up my paramedic patch (I run IT for our EMS organization), I still get the same feeling you get when I hear stories about how the entire EMS continuum from 9-1-1 assisted (or not) bystanders to first responders, transport, and eventually hospital comes together to save a life. Even though I’ve done this for 25 years, I can still tell you just about every save that I’ve been a part of (and the babies delivered too). Funny, those good sorties always seem to stand out and the sad ones fade away over time.
Well done to all!
—
Yeah, I vividly remember the only birthin’ baby call I had, but it was particularly memorable: it’s the only baby born at San Quentin prison! But that’s a whole other story…. -rc
I have to disagree with your comment about a-fib not being as serious as v-fib.
Having had a-fib myself, it can be a killer. One attack caused me to pass out and smack my head on the concrete. Another attack had my heart beating at over 360 beats a minute. As you well know, at 360 BPM NO BLOOD moves through the heart so it is the equivalent of the heart completely stopping. Needless to say, without blood circulating you have a couple of minutes before your brain dies.
When the EMS folks arrived (luckily EMS responds within 5 min or less around here) they had to give me three shots of the med that supposedly suppresses a-fib before it took effect. If the third one didn’t work they would have had to crack my chest to fix my heart.
Luckily, a-fib is correctable by burning the node that is issuing the false signals to the heart that control the pace of heartbeats.
I had that operation and other than waking up in the middle of the operation as they were burning (with an electrical probe sent up through my groin while the camera was sent down through my carotid artery) the node on my heart (which really hurt bad but the anesthetic prevented me from moving or speaking out to tell them I was awake), it fixed the problem.
The surgeon told me I was dreaming about being awake until I repeated verbatim the gossip he was telling the anesthesiologist about several other doctors when I was supposed to be “out”, which confirmed I was indeed awake and embarrassed the heck out of the surgeon!
—
I’ll bet. I didn’t say a-fib was completely innocuous, but it is far less serious. If not corrected, v-fib leads to death in minutes every time, while I know many people who continue to function reasonably well with a-fib. That’s pretty much the most extreme difference of “serious” available. -rc
This is the daughter who started the CPR on my dad. I just wanted to Thank you again for doing what you do. You truly made a difference that early Sunday morning. I’m emotional reading the story and even thinking about it. I’m so thankful you both got there as quickly as you did despite going down the wrong driveway. When I’m done with nursing school I hope to come there and work and be close to my family. Keep up the good work.
—
Hi Becky. I’m sure your mom told you about this page — we had a nice visit with her and your dad today. They asked a lot of questions, and filled in some details for us. Your parents are great people, and I hope we can welcome you and your husband to the area soon. -rc
Thanks for that story. My best friend’s brother died on the floor of a supermarket surrounded by people who didn’t know CPR while they waited for an ambulance to arrive. So thanks again for the uplifting story. It made my morning.
Couple of thoughts. First, 10 years on the street, and the number of times I was thanked by family was in the 10% range, but I agree: The stress of the moment, and being in a larger city environment, didn’t lead to thanks. And then again, I didn’t do it to get thanked (but it was nice when it happened).
Second, having spent a few years in-hospital, doing cardiovascular research, rapid defibrillation is a key element to survival. But effective CPR is wonderful. Becky, you did good. Whoever taught you how to do CPR did good, too.
Dale, your experience in the cath lab during ablation is one I’m sorry to hear about. Something like that’s stressful, and not what you needed at that point. Wish they’d dialed up the drugs a little bit and let you forget it all!
And finally, Randy (everyone else stop reading), I guess an 18’s better than a 22 butterfly, but real men use a 14 for a cardiac patient! 😉
—
I’m pretty sure a 14 wouldn’t have fit the vein that popped up. I figured a patent 18 was better than a blown vein, so that’s what I went for. I looked for another one on the other arm on the way in, but nothing presented itself. -rc
First Responders such as you are a Godsend in rural areas. When I was an EMT in Staunton (STAN-TON) Va in 1985, we had TWO calls come in at the same time. One, a shortness of breath and the other for a nursing home that said they had the patient on Oxygen (Which usually meant they were doing CPR). We sent First Responders to the Shortness of Breath and we took the nursing home call. The calls were in OPPOSITE ends of the county. The nursing home call was routine, but the First Responder call was a FULL CODE when they got there. 47 minutes later, we arrived to administer the FIRST shock. To our amazement, we got a good pulse. The guy went home on Christmas Eve and is STILL alive today 24 years later! I take NO credit for his save, it was the First Responders who saved this guy’s life. I’ll never forget this call.
—
Man: 47 minutes is an eternity to do CPR, and it’s amazing you got him back. Awesome! But it figures: you were probably bored all day, and then got two at once. Fate seems to like to pull that one! -rc
As a Hospital Corpsman in the Navy I understand what you did and the importance of your educational efforts here. I’m really glad that things worked out for your patient. Most of my emergency experience was in Vietnam so I was usually not able to follow the patient as long as you have here. I will tell you that, even more than 40 years later, I sometimes wonder how some of them did later.
Good work!!
I deliver newspapers at night in rural, semi-rural, and sub-urban areas. I can give people some tips regarding making your address markers visible. HIGH-CONTRAST — do not use brass numerals; they just reflect glare; use black characters on light paint, and vice-versa. Do not place the numerals more than eight feet above the ground. Do not place the numerals immediately around a porch light; there will be glare, or, often times, a shadow right where the numbers are. Be sure to look at your numbers at night, so you can tell how visible they are.
Be sure that your numbers are not obstructed by shrubbery or other items. The larger the characters, the more legible they are!
A guideline: if you had an emergency, could EMS find you?
I’m a workplace first-aider, and required to CPR-AED, which had been somewhat of a waste of time until recently, when my workplace finally installed an AED in our building lobby. This is a little bit of a pain, as it’s 3 floors below the lowest office, but it puts it in a public place, so it’s not just for our employees. Thankfully, I haven’t needed it yet, but forewarned is forearmed.
The community hackerspace I help run has been talking for too long about a first-aid/CPR class, and I think this story might be the impetus we need to actually get in touch with the local medics and put something on the schedule. I’ve taken the training for work, since I’m around electrical equipment all day, but I want to know that our other members have learned it, too!
It’s a shame that the Rock Band drum pads are AC-coupled and wouldn’t resolve the relatively slow (>1ms) rise-time of a chest compression, because the game logic definitely already knows how to critique one’s tempo! Can you imagine if every gamer kid learned CPR as early and as thoroughly as they learn zombie-blasting? I see much hack potential here….
—
I like the way you think! A world-useful hack. And yeah: time to stop talking about it, and just do it. -rc
Many places in Australia now use what they call the Rural Numbering scheme.
This has star picket (fence post) with a black plastic top piece with reflective numbers on it. It is based on the road distance of the property entrance way in metres x10 from some particular landmark. Slight inaccuracy is allowed so two properties can have adjacent numbers if necessary even if they share an entrance way.
This is great because the numbering allows emergency services quick location of properties & the numbering uses a standard basis. Being metric here, where a kilometre is 1000 metres, it is easy to work out a location. If you see number 300 & you are looking for number 600 then you know you have 300 metres x 10 = 3 kilometres to go.
It could be converted to yards & still use the metric system ie you see number 300 & you are looking for 600 then you know you have 3000 yards to go. Just not quite as convenient.
The idea of having every property marked with a standard system works very well. Some councils even paid charities to install the posts. They were paid a set fee for each post done & it only required a vehicle that could fit the posts & the post rammer. It was not a difficult job & the money went back to the community.
—
Our county also uses distance along a road to assign addresses, but as you note (and as we have found!), even on a rural road there can be two houses fairly close together. So you know you’re in the right vicinity, but which house is having the extreme emergency where they need intervention RIGHT NOW or someone is going to die? So yes, the houses need to be clearly marked in a way that can be seen by a blurry-eyed ambulance crew at night if you expect help. Isn’t it worth the effort to do that before it’s needed? Because you won’t have time once the emergency is in your face. -rc
Living in a rural area in Virginia, I joined a service group called Ruritans. As one of our projects, we have placed AEDs — Automated External Defibrillators — in several public places open 24/7, and informed folks that these are available for emergency use. Clear graphic instructions are printed on these devices so anyone can use them, no training required.
—
That’s great, since that increases the odds of survival dramatically. But training is required, in that defibrillation isn’t enough; effective CPR is a must before and after. CPR classes do have a section on AEDs to ensure it’s done correctly, because you’re in a true life or death struggle and you want to get it right. An AED is absolutely NOT a replacement for training. -rc
Congratulations on the job you did. I worked for twenty years as an on road paramedic in Tasmania and managed to archive a few, very few, true saves from Cardiac Arrest. You’re right when you say that competent CPR followed by early defibrillation is the best possible treatment.
My wife (retired GP) and I were recently in the UK and noticed that with the proliferation of mobile phones there is no longer a need for the old red public phone box that used to be so common. What we also noticed is that these same old red phone boxes have not been removed but now contain AEDs (Automatic External Defibrillators) along with instructions for CPR and how to use the AED.
I thought it was the best idea I had seen in a long time and it obviously has the potential to save lives.
—
Neat! I’m afraid that here, though, they’d all be destroyed in a week by vandals (sigh). -rc
From asleep to on the road in a minute? That’s scary good. Impressive.
—
We couldn’t always do it, but often did. It was helpful that night. -rc
First time someone introduced me to a loved one as “the guy who saved [her] life” it freaked me out. I had to change the way I thought about who I am.
—
It’s quite a privileged title, isn’t it? -rc