The first two stories this week have brief summaries of two different court orders: you might utter a distressed “You can’t be serious!” on one. The other could be described with the same words, but with an opposite emotion.
Fight the System or Die Trying
A 19-year-old teen identified only by the initials “ST” is dying from mitochondrial depletion syndrome — a genetic, degenerative disease that has been destroying every part of her body: sight, hearing, muscles, bones, kidneys, and lungs. But it doesn’t affect her brain, and she’s asked to travel from the United Kingdom to Canada, where a medical trial has a very slim chance of saving her life. “This is my wish,” she said. “I want to die trying to live. We have to try everything.” Two hospital psychiatrists determined she has the mental capacity to make her own decisions, but the British National Health System — and a judge — disagree. “I find on the balance of probabilities that ST’s complete inability to accept the medical reality of her position … is likely to be the result of an impairment of, or a disturbance in the functioning of, her mind or brain,” the judge said. The decision is the first step in approving the NHS Trust’s request to move ST into palliative care, which among other things would remove her from dialysis — ensuring her death from kidney failure in a few days. Also, she’s known as “ST” because of a standing court order for her to remain anonymous. “We are not allowed to ask people for prayers or for help which she desperately needs,” ST’s family said in a statement. “It is a matter of life and death for our daughter to raise money for treatment in Canada, so these arbitrary reporting restrictions are literally killing her. We are shocked to be told by the judge that our daughter does not have capacity to make decisions for herself after all the experts have said that she does.” (MS/London Telegraph) …When she said “die trying” she probably didn’t think it would be in court.
Publisher’s Comments
True contributor Mike Straw, who wrote this story, was not aware when he wrote it that ST has died. Her family issued a statement via Christian Concern that “On Tuesday evening [Sept. 12] we lost our beautiful and courageous daughter, known to the world as ST. To us she has a real name. Even now, in the hour of our grief, we continue to be gagged by the court order from saying her name aloud.”
They note that “ST was a committed Christian and firmly believed that life is the most precious gift we have from God. Every family faced with such a challenge and tragedy should have the opportunity to leave no stone unturned when trying to save the life of their child.”
Christian or atheist, it’s hard to argue otherwise, yet Britain’s National Health Service did just that.
The NHS is not just a conglomerate of government-funded hospitals and clinics, it’s essentially what Americans would call a “health insurance” company or, more accurately, an HMO. So another way to look at this is that the insurance company not only wants to “pull the plug” to save money, but it asks a court to shield it from disclosure of what hospital, what doctors, and even the patient’s and family’s very names. That meant the family had significant barriers to, say, create a GoFundMe page to help collect money to pay for the young woman’s treatments abroad.
 If that doesn’t give you pause, it should.
If that doesn’t give you pause, it should.
The web site notes that on Sept. 22, the family will “appear at a hearing in the Court of Protection to ask for the reporting restrictions to be discharged and for them to be given a right to tell their story.” It seems reprehensible to have made the order; it would be more so to not grant that request.
Once I saw Mike’s story last night, I alerted him that I’d be blogging about it (and the other court decision, following), and asked if he had anything he’d like to add. He certainly did:
Mike Straw’s Comments
This story hit me differently compared to most of the stories I write for True. Like many people, I feel a lot of anger about the whole situation, but that anger is broadly focused and tempered with the understanding that comes with personal experiences.
My wife, Deanna, has an uncanny ability to understand the end-of-life process differently from most people. As clergy, her favorite thing to do is funerals — we often joke that she puts the “fun” in “funeral.” Recently she started volunteering at a local hospice, so the idea of allowing someone to die at their time in the way they desire is on our minds a lot lately.
I’ve also learned more about that process having her around, including deeply personal experiences when my uncle and her mother died while under hospice care. She was able to explain what was going to happen and shed light on things that had happened, including our grieving processes. Death affects everyone in very powerful ways, and that power can be seen in how different people are processing the then-future and now-past death of this one young woman.
This article takes the positives of hospice, palliative care, and end-of-life decisions and flips them on their head. And it does that because of the one thing these all need: the recognized humanity and autonomy of the person who’s dying.
I get most angry at this particular sentence from the judge: “In my judgment, and based upon the evidence which is now before the court, I find on the balance of probabilities that ST’s complete inability to accept the medical reality of her position, or to contemplate the possibility that her doctors may be giving her accurate information, is likely to be the result of an impairment of, or a disturbance in the functioning of, her mind or brain.”
Modern psychology has come to understand that we are not persuaded by facts, but by emotions and subconscious biases. It’s only after our subconscious minds have made a decision that our conscious minds find the facts to boost what we’ve already decided, and discard facts that contradict it.
(For some great plain-English explorations of this idea, I found the book The Righteous Mind: Why Good People Are Divided by Politics and Religion by Jonathan Haidt, and David McCraney’s You Are Not So Smart podcast, to be very helpful.)
You can see that here: the judge seems to have some strong biases for removing life-saving care when it’s no longer likely to help. That bias may be financially motivated (as the NHS is incurring significant costs keeping her alive), or it may be motivated by compassion and not wanting to see ST continue to suffer unnecessarily, or it may be a combination of these and other motivations. Whatever the motive, the fact that “my judgement” that is “based upon the evidence” is so contrary to the evidence shows that there is definitely a bias there.
This question was very complex, and there was never a “good” answer, but like so many other things in this world the “best” answer would have been to respect ST’s wishes and grant her the right to choose how she dealt with her own mortality and how much she chose to fight it.
ST never seemed to have misunderstood the facts of her horrible disease or have any illusions about how likely it was that the treatments would work. She just wanted to make a final stand against the disease and either win or go down fighting. This isn’t delusional or a sign of “an impairment of, or a disturbance in the functioning of, her mind or brain.” It’s a sign of someone wanting to have some control over how she went out.
We had some confusion in our home for a bit about the use of the term “palliative care”. The way it’s used in this case is different from Deanna’s understanding. It wasn’t until I saw a bit in the Wikipedia article on palliative care that I understood why. In the United States, palliative care and hospice care are different.
Deanna said, “Hospice is enabling the patient to have a choice in the way in which they receive end of life treatment. Its root is important because we keep the patient as comfortable as possible, giving them all choices within their control. If they wish to get treatment to make them ‘better’ they are discharged from hospice and receive palliative care.” But as Wikipedia points out: “In the common vernacular outside the United States, hospice care and palliative care are synonymous and are not contingent on different avenues of funding.”
I think the way we define palliative care in the U.S. would have been perfect for ST.
[End of Mike’s comments]Alexander Cohen’s Comments
Alexander is the other True contributor. He didn’t write this one up for True, but he did for his own publication on Substack. See She wants “to die trying to live.” on Substack.
Download the Court Decision
This one is fairly dense compared to the other case below, but I want it to be available so those who want the best chance of understanding the decision can read the judge’s words directly and fully. I’ve only had time to read the first few pages, and barely skim the rest.
Craven Disregard
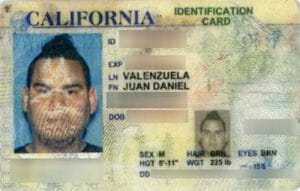 Juan Valenzuela, a prison security guard in Colorado, went through security at Denver International Airport in February 2017. He presented his I.D. — an expired California Identification Card — but the TSA agent thought it was suspicious. Valenzuela explained it had been damaged by a trip through a washing machine and provided more I.D., including his Social Security card, his government-issued work photo I.D., and his firearms certification card, which also bore his photo. But the TSA agent summoned Denver police, who arrested Valenzuela for “forging” a government document, a felony. A prosecutor “took one look” at the case, noting the washed card still had its security features intact, and dismissed the charge. That took several months, and Valenzuela was struggling to pay rent and feed his family after being fired from his job. He eventually got his job back, and not surprisingly, he sued. In 2022 a federal court awarded Valenzuela $200,000 in compensation plus $300,000 in punitive damages against Karl Coleman. Coleman is the Denver police officer who swore out the complaint even after doing a records search and finding Valenzuela had a valid California driver’s license bearing the same number as the I.D. card. The court found his actions “reprehensible,” and also ordered the Defendant to pay Valenzuela’s lawyer’s $485,200 legal bill. Still, there were apparently unsettled issues, perhaps including that DPD officer Ligela Craven had called Valenzuela’s boss at the prison, who confirmed Valenzuela’s identity, but went ahead with the arrest anyway. Last week, the Denver City Attorney recommended the city settle the remainder of the case and award Valenzuela an additional $825,000. (RC/Denver Post) …Also reprehensible: that it takes more than six years to settle such an open-and-shut case.
Juan Valenzuela, a prison security guard in Colorado, went through security at Denver International Airport in February 2017. He presented his I.D. — an expired California Identification Card — but the TSA agent thought it was suspicious. Valenzuela explained it had been damaged by a trip through a washing machine and provided more I.D., including his Social Security card, his government-issued work photo I.D., and his firearms certification card, which also bore his photo. But the TSA agent summoned Denver police, who arrested Valenzuela for “forging” a government document, a felony. A prosecutor “took one look” at the case, noting the washed card still had its security features intact, and dismissed the charge. That took several months, and Valenzuela was struggling to pay rent and feed his family after being fired from his job. He eventually got his job back, and not surprisingly, he sued. In 2022 a federal court awarded Valenzuela $200,000 in compensation plus $300,000 in punitive damages against Karl Coleman. Coleman is the Denver police officer who swore out the complaint even after doing a records search and finding Valenzuela had a valid California driver’s license bearing the same number as the I.D. card. The court found his actions “reprehensible,” and also ordered the Defendant to pay Valenzuela’s lawyer’s $485,200 legal bill. Still, there were apparently unsettled issues, perhaps including that DPD officer Ligela Craven had called Valenzuela’s boss at the prison, who confirmed Valenzuela’s identity, but went ahead with the arrest anyway. Last week, the Denver City Attorney recommended the city settle the remainder of the case and award Valenzuela an additional $825,000. (RC/Denver Post) …Also reprehensible: that it takes more than six years to settle such an open-and-shut case.
To get this out of the way first: I can’t help but wonder if Hispanic security guard Juan Valenzuela had been an executive-level white guy with a name like, say, Gordon Studebaker III, would he still go to jail for a washing machine-damaged I.D. card backed up by other officially-issued photo I.D.s?
Let’s just say I doubt it.
It’s bullying and outrageous (“reprehensible”) conduct, and the police must be slapped again and again and again if necessary to get it through their skulls that their job is “to protect and to serve” with discretion and intelligence, not to beat on people — literally or figuratively — because they are brown. The sad part is, taxpayers have to pay for such settlements, so we all really need to work to demand better from the governments we pay for.
Download the Court Decision
Anyway, what’s of most interest to me is the final court order from 2022, the facts from which were used by the reporters of the source stories I used to briefly tell you what happened. The defendant(s?) had made several post-trial motions trying to squelch punitive damages, trying to not pay Valenzuela’s lawyer fees, trying again to claim immunity, etc. In her Order, the judge analyzed each point and shot them down beautifully, one by one. I, at least, found it very interesting reading.
ST 23 September Update

The gag order was lifted on 22 September, and it was revealed that “ST” is Sudiksha Thirumalesh. Victoria Butler-Cole KC, the lawyer for the NHS Trust involved, said the Trust had “no objection” to the now-dead 19-year-old to be named. But which NHS Trust was involved in fighting all of this? That is still part of the gag order!
“This profoundly disturbing case has demonstrated the urgent need for an overhaul into how end-of-life decisions are made in the NHS and the courts,” said Christian Legal Centre CEO Andrea Williams.
(Source: BBC)
– – –
Bad link? Broken image? Other problem on this page? Use the Help button lower right, and thanks.
This page is an example of my style of “Thought-Provoking Entertainment”. This is True is an email newsletter that uses “weird news” as a vehicle to explore the human condition in an entertaining way. If that sounds good, click here to open a subscribe form.
To really support This is True, you’re invited to sign up for a subscription to the much-expanded “Premium” edition:
Q: Why would I want to pay more than the minimum rate?
A: To support the publication to help it thrive and stay online: this kind of support means less future need for price increases (and smaller increases when they do happen), which enables more people to upgrade. This option was requested by existing Premium subscribers.

13 years of the Reich of Tories have destroyed the spirit and finances of the NHS. Not the best in the world nor the first national health service ever. Certain decisions are taken at higher levels by the Reich of Tories lackeys or backers to spend less money on care on the public. Always remember this Reich of Tories (united kingdom of great britain) has the second largest unelected parliament in the world, second only to China.
When ST said she wanted “to die trying to live,” she was speaking to a psychiatrist who was evaluating her for the court. She seems to have been confident the court would decide in her favor, but she did at least know that fighting in court was going to be necessary.
I think ST also recognized that participating in this medical trial, while it might not save her, had the possibility of providing information that could help in the saving others with this syndrome. So the judge and the NHS are guilty of prolonging the suffering of others and probably cost the NHS more money in the long run.
Re ST — contrary opinion. I don’t see any obligation on the part of the NHS to pay for a patient to get into a medical trial in another country when the medical trial has very little chance of working. If she and her family could pay her own way, that would be different. But chasing after extreme solutions at end of life that are unlikely to work — that actually is driving up costs for all of us. Jahi McGath, Terri Schiavo — we’ve seen these kinds of cases before. Yes, in this case the patient had her own agency. And yes, if she could have paid her way — great. But since the trial was unlikely to cure her … should the NHS pay her way? I don’t know why the judge said she didn’t have the mental capacity to make her own decisions. Maybe that was a legal thing.
It’s always hard when it’s personal. I read a story years ago about a baby who could not live unless connected to various machines. He spent his first year in the hospital, hooked up 24X7. One of the parents wanted to bring him home; the other wanted to keep him in the hospital. I don’t know how it turned out but wow — the expense! but if it was my baby I would say do whatever you can! but a life on machines from the day he was born — wow. But who am I to say it’s not worth it? Complicated issue. Oh, that case was in Britain. So they do provide long term care for at least some patients.
—
My reading wasn’t that the family wanted NHS to pay for a trip to Canada or experimental treatment there; they were clearly ready to do fundraising for that. They just wanted NHS to not stop with the treatments to keep her alive until that fundraising was far enough along to get ST to Canada, but the NHS didn’t want to simply keep her on kidney dialysis. Seems mean-spirited. -rc
Look at past cases, this isn’t anything new, and it isn’t a matter of NHS paying today, but they actively prevent people from getting medical assistance elsewhere. Likely it is because if the person lives, then NHS would be forced to pay for treatments in the future and they really don’t want that to occur. It is far better for them to have people die. This is what you get with government run “health care”, they don’t care, it is all about how they look and money. What I mean by how they look is if the person gets care elsewhere and lives, then they look bad, but if the person dies, then they look fine as they say there was nothing that could be done and you can’t prove otherwise.
You think private healthcare with their automatic denial of paying for treatments because it cuts into their bottom line is any better?
What they denied ST was Kidney Dialysis . I am familiar with this as I had a neice who died last year after over 7 years on dialysis. It is relatively cheap. Easy to do at home. My brother and his wife did it for most of those seven years. Neither of them are medical professionals. To me it is the same as denying food or just throwing a pillow over her face as this is a basic biological function they denied her assistance to perform. I don’t know how long ST could have lived with that disease. All indications were not long, but, was that a month, years? Time ST could have used to come to terms with what was to come. At minimum, some time could have been granted to allow extended family to get there to say goodbye and perhaps pursue private sources of dialysis at their own expense.
To tell you what death from lack of dialysis is like, within just a few hours, you are groggy and in an altered mental state as the toxins build up. You are asleep within 12-16 hours if not before. This is a sleep you never awaken from. There are no goodbyes. It is a short window and you are effectively gone, the dying just takes longer, up to 36 to 72 more hours. Literally within a few hours of her being denied care, Her parents watched her eyes close for the last time. For a few hundred dollars, they could keep her alive another week or even a month.
I think I saw somewhere that a dialysis patient costs about $12 a day to keep alive. They could have revived her with dialysis up to a couple of hours before death. From the articles I suspect she had already been unconscious when the court issued it’s ruling. So they may not HAVE said goodbye, hoping the court would save her. The price of a good sit down meal at a nice restaurant could have woke her up and let her say goodbye.
Obviously her underlying condition couldn’t be treated, but this is no different that denying a Covid patient a vent or oxygen to breathe. Or someone suffering from thirst a drink of water or starvation, food. It’s we think your situation is hopeless, so we are going to hasten you along. Literally.
Here is the sad thing to me. I think Obamacare and our new system will eventually become what NIH already is. What prevents it from being that already is that there are still private providers out there. One of which saved me by performing a very expensive heart operation for basically free or next to nothing. But as the budget becomes more of a problem and cost cutting starts coming they will chip away at the private entities and replace them with state ones. Then there will be no second opinion. Then when they think you are no longer worth having, they will cut off one of your basic functions, food, water, air or waste. And you will die quietly if not quickly. I doubt I will live to see it, with my health prognosis.
But, 10, 15, 25 years, I think people will regret what they have done. Today, we can appeal to a charity. We can start a gofundme. When there is only one provider, we will all be ST. The formula will decide if we live or die. Even our death row inmates get more consideration from our government than an innocent woman was given by theirs. There is a REASON our founders sought to limit what powers that our government had.
Kudos for pulling the actual court decisions — too few people actually do that, and news reports, while often accurate (at least in the sources I read), are rarely complete. Also, I’ve sometimes found that the headline doesn’t agree with the article (authors don’t write the headlines), and sometimes the author gets it wrong too!
A few years back in the US there was much talk of “death panels”. There have ALWAYS been death panels in one form or another, Insurance Companies/Limits being the primary one.
In the case of ST I got the impression that she was not asking the NHS to provide payment (except possibly for transport, not a large amount) for the Canadian study (which are almost by definition free) but simply the right to try.
The gag order is what is reprehensible, a GoFundMe page or the like would likely have resulted in her travel and accommodations being taken care of.
Lastly, on this topic, I don’t think there is a single perfect answer. As near as I can tell no medical system is perfect, at least not as regards major health issues. Minor health issues like colds, vaccines, etc seem to be handled pretty well by all health systems.
On the second story regarding the washed drivers license I believe this might have been 1) outright racism (the most likely), 2) too many people gaming the system and too little resources.
I tend towards the racism as it seems they had obtained ample evidence to let the guy go while at the airport, at most having to take a later flight.
I hope there is follow-up on this as the people involved, especially the supervisor, should be fired. THAT is how you send the message to the rank and file to behave correctly.
I had actually saved these two stories to comment to Randy personally but thanks to this blog entry I can do it here. As always, Randy et al, thanks so much for what you do.
—
Thank YOU, Andy, for helping to make it possible with your Premium subscription. -rc
Doctors should be willing to try to do everything possible to save a life, instead of taking the easy way out, as these doctors did. She deserved the chance to try the alternative treatment that was denied. This story says much about the NHS in the UK (and it’s not good). Sad story!
This was a decision by _administrators,_ not doctors, as far as I know. The NHS has become a hell-hole of bureaucratic monsters, as witness the ongoing disputes between government and medical staff who just want to be paid fairly.
A National Health Service is an admirable standard — some would say an absolutely vital one — to aspire to but laziness and selfish greed will sooner or later find a way to become the uppermost factors in decision-making and then you end up with this kind of utterly mean, sociopathic ruling.
George, you are entitled of course to you opinion, but can I suggest that you look at infant mortality rates, longevity and access to health care indicators in health care systems in Europe against those of the US and see if that says much about the US health care system. People die every day in the US because they cannot even get access to the system, such as not being able to afford basic needs such as insulin. ST’s death was inevitable and trial in Canada that she pinned her hopes on had ended. The number of people dying in the US due to lack of adequate healthcare which is not inevitable but a political choice to allow people to die on the basis of their ability to pay is looked on with horror by the rest of the world.
Having now seen that “ST” is Sudiksha Thirumalesh, and seen her picture, I can’t help but wonder if the outcome of this case would have been different if “ST” had stood for something like Samantha Tucker.
It’s possible, but unlikely, I suspect. The UK in general, and the NHS in particular, has become very diverse (a statement based on anecdotal evidence and confirmation bias, to be sure!)
There are a number of points that appear to have been omitted from the reporting, here:
The Canadian trial was not available, so the case was about the move to palliative care.
Mrs Justice Roberts noted, before ruling in August that ST should be moved to palliative care, that the Canadian trial had ceased operating as it had lost/run out of funding. So the, much touted miracle, was not available.
ST had not been moved to palliative care because there was an appeal ongoing, but passed away none the less.
Victoria Butler-Cole KC observed that the reporting restriction referred only to the legal proceedings, not to any potential fundraising activities. So, if that was the advice that the family of ST were given, it was really, really, bad. Whether this would have been due to incompetent, or an organisation acting in their interest, rather than the family or ST’s, is unknown?
I’d also note that no estimate of the cost of transporting ST to Canada, or the cost of participation in the trial has been made. The transport alone would be eye-watering for a patient on a ventilator, experiencing severe health incidents on a daily basis.
The comparison of the NHS to any aspect of the US health-care system is incorrect, and makes it clear that you don’t understand the NHS. There are no CEOs, no corporations and no profits. The NHS budget is spent to get the best outcomes based on priorities of need, urgency, and outcome (likely benefit).
The tragedy that this young girl got an incurable disease is only compounded by those who exploit the family’s desperate hopes for their own ends.
Exactly so. There is much in the reporting of this case which manipulates the facts to support an anti-NHS agenda and a political opposition. The attempts to simplify or clarify how the system works by creating false anologies with the US health insurance/HMO system is misguided at best.
What is most reprehensible about Valenzuela’s story is his lawyer’s $485,200 legal bill.
—
On the one hand, it has been 6-1/2 years to get to this point. On the other hand, I’ll bet that isn’t the final total. -rc
I was in two minds about whether to engage with this debate, because a lot of the answers clearly do not understand the structure of the NHS and ignorance of how the Court of Protection works. The NHS is not remotely analagous to a US HMO or medical provider and I say this as someone who has worked in the health system in the US and UK and actually worked for an HMO. The safeguarding processes of the NHS are inadequate for situations like this and need to change but the narrative that financial considerations had anything to do with this decision are far off the mark. First, the treatment offered in Canada (and also in Italy) was not at the expense of the NHS or the UK Government. If anything, there was a financial dis-incentive for the NHS to oppose the patient’s transfer out of the system.
The Court of Protection’s default position is one of confidentiality, because it’s sole purpose is to make decisions where there are vulnerabilties and questions of about individual’s mental capacity. The same applies to records in the US court’s relating to juveniles for example. People have quite rightly questioned the judge’s decision to disregard the psychiatrists (who are also from the NHS) who advised the court that she had capacity… but all judicial systems are flawed and subject the these issues. In the end, judges are the independent arbiters in every democratic system of government, including the US. Sadly, she died before an appeal could be launched.
The judicial system is NOT the government and it was not the government and the NHS against the patient. The doctors within the NHS do not benefit financially from withdrawing treatment from patients and there are detailed and clear safeguards in place to prevent the NHS from making these decisions for financial rather than humanitarian or best interests reasons. The fact that this got to the Court of Protection was precisely because those safeguards are in place. It was NOT the decision of the NHS to withdraw treatment. It was the RECOMMENDATION of the doctors to do so, and the Court of Protection after reviewing the medical evidence and the family and person who made the decision. The Court of Protection, in refusing to name the hospital involved is trying to protect doctors from being blamed for the decisions taken by the Court of Protection and the judge. The judge took the decision the judge’s name is in the public domain.
Having said that, there is a culture within the Court of Protection of secrecy/confidentiality which needs to change and the criticisms are legitimate. There is also a culture with the Court of Protection which at times is over patrician and gives insufficient regard to the individual’s rights to make decisions, even bad ones. The Mental Capacity Act of 2005 tried to address this, but more work needs to be done to have open justice and change in culture within the courts. Lastly, the description of the role of “Christian Concern” in this process implies they are a benign organisation trying to help a poor patient against a monolithic health system. Christian Concern and its sister organisation the Christian Legal Centre has some very illiberal positions on abortion, human rights, anti Islam and on homosexuality, far outside the political mainstream of the UK and has questions to answer about exactly where their funding comes from. I think the decision of the judge was wrong and our court of protection system does not serve people in these situations well. However, some of the sweeping and misguided commentary on this case is just plain wrong and some of the people making this commentary have other agendas which have nothing to do with compassion and a desire to help ST.
—
Thanks for weighing in with more “insider” information.
I brought in HMOs so readers who have no idea what the NHS is could have a frame of reference, as the vast majority are American. I perhaps used too few words, so I asked ChatGPT to make the comparison “in one paragraph.” The result:
-rc
I don’t disagree with the AI comparison! I haven’t engaged much with the AI tools out there, but I’m pretty impressed!
—
There is definitely promise, though I’ve blogged on the caveats about AI last December and in June. -rc